Prognostic Factors of Survival in Veno-Arterial ECMO Patients: A Multivariable Logistic Regression Analysis
DOI:
https://doi.org/10.5195/ijms.2023.1557Keywords:
Survival, Veno-Arterial ECMO, Multivariable Logistic Regression Analysis, Critical care, Resource allocation, Ethical discussions, Patient selection, SAVE score, Hemolysis, Inflammation, Risk prediction model, Mortality, Smoking, Dialysis status, BMI (Body Mass Index), Atrial fibrillation, Hypertension, Diabetes mellitus, COPD (Chronic Obstructive Pulmonary Disease), History of cardiac arrest, Retrospective study, Single-center study, Provider bias, Stepwise model selection, Logistic regression, Clinical endpoints, ExplantationAbstract
Background: Several models exist to predict mortality in patients on Veno-arterial (VA) extracorporeal membrane oxygenation (ECMO). Whether expanded demographic data points have prognostic implications is less understood. This study assessed the prognostic value of demographics in patients on VA-ECMO.
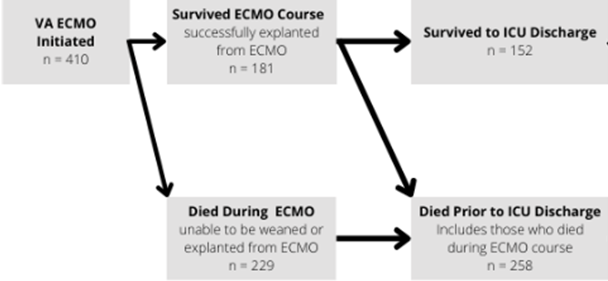
Methods: This retrospective cohort study investigated 410 patients who received VA-ECMO. Survival to hospital discharge, survival to intensive care unit discharge and survival to ECMO explantation were examined. A multivariable logistic regression was performed incorporating 11 demographic variables.
Results: 44% (181/410) of patients survived to ECMO explant, 37% (152/410) of patients survived to ICU discharge, and 36% (146/410) of patients survived to hospital discharge. There was an increase in odds of survival to hospital discharge in patients who were less than 55 years old (Odds Ratio (OR) = 3.91 [95% Confidence Interval (CI) 2.35-6.49]). There was a decrease in odds of survival to hospital discharge in patients who had a prior cardiac arrest (OR = 0.35 [95% CI 0.20-0.63]). Patients who survived to hospital discharge less frequently had a history of smoking (51% vs 65%, respectively; p=0.008), and were younger compared to those who did not survive (51.4+/- 14.03 vs 57.3+/- 16.54).
Conclusion: Age less than 55 years old was a prognostic indicator of survival to hospital discharge following VA-ECMO, while history of smoking, history of dialysis, and history of cardiac arrest were associated with mortality. Sex, BMI, atrial fibrillation, hypertension, DM, and COPD were not significant indicators. These data may help guide optimal patient selection for VA-ECMO support.
References
Chakaramakkil MJ, Sivathasan C. ECMO and Short-term Support for Cardiogenic Shock in Heart Failure. Curr Cardiol Rep. 2018;20(10):87. DOI: https://doi.org/10.1007/s11886-018-1041-4
Paolone S. Extracorporeal Membrane Oxygenation (ECMO) for Lung Injury in Severe Acute Respiratory Distress Syndrome (ARDS): Review of the Literature. Clin Nurs Res. 2017;26(6):747-62. DOI: https://doi.org/10.1177/1054773816677808
Telukuntla KS, Estep JD. Acute Mechanical Circulatory Support for Cardiogenic Shock. Methodist Debakey Cardiovasc J. 2020;16(1):27-35. DOI: https://doi.org/10.14797/mdcj-16-1-27
Guglin M, Zucker MJ, Bazan VM, Bozkurt B, El Banayosy A, Estep JD, et al. Venoarterial ECMO for Adults: JACC Scientific Expert Panel. J Am Coll Cardiol. 2019;73(6):698-716. DOI: https://doi.org/10.1016/j.jacc.2018.11.038
Hoyler MM, Kumar S, Thalappillil R, White RS, Tam CW. VV-ECMO usage in ARDS due to COVID-19: Clinical, practical and ethical considerations. J Clin Anesth. 2020;65:109893. DOI: https://doi.org/10.1016/j.jclinane.2020.109893
Murugappan KR, Walsh DP, Mittel A, Sontag D, Shaefi S. Veno-venous extracorporeal membrane oxygenation allocation in the COVID-19 pandemic. J Crit Care. 2021;61:221-6. DOI: https://doi.org/10.1016/j.jcrc.2020.11.004
Giraud R, Legouis D, Assouline B, De Charriere A, Decosterd D, Brunner ME, et al. Timing of VV-ECMO therapy implementation influences prognosis of COVID-19 patients. Physiol Rep. 2021;9(3):e14715. DOI: https://doi.org/10.14814/phy2.14715
Hong X, Xiong J, Feng Z, Shi Y. Extracorporeal membrane oxygenation (ECMO): does it have a role in the treatment of severe COVID-19? Int J Infect Dis. 2020;94:78-80. DOI: https://doi.org/10.1016/j.ijid.2020.03.058
Schmidt M, Burrell A, Roberts L, Bailey M, Sheldrake J, Rycus PT, et al. Predicting survival after ECMO for refractory cardiogenic shock: the survival after veno-arterial-ECMO (SAVE)-score. Eur Heart J. 2015;36(33):2246-56. DOI: https://doi.org/10.1093/eurheartj/ehv194
Chen WC, Huang KY, Yao CW, Wu CF, Liang SJ, Li CH, et al. The modified SAVE score: predicting survival using urgent veno-arterial extracorporeal membrane oxygenation within 24 hours of arrival at the emergency department. Crit Care. 2016;20(1):336. DOI: https://doi.org/10.1186/s13054-016-1520-1
Smith M, Vukomanovic A, Brodie D, Thiagarajan R, Rycus P, Buscher H. Duration of veno-arterial extracorporeal life support (VA ECMO) and outcome: an analysis of the Extracorporeal Life Support Organization (ELSO) registry. Crit Care. 2017;21(1):45. DOI: https://doi.org/10.1186/s13054-017-1633-1
Bateman RM, Sharpe MD, Jagger JE, Ellis CG, Solé-Violán J, López-Rodríguez M, et al. 36th International Symposium on Intensive Care and Emergency Medicine : Brussels, Belgium. 15-18 March 2016. Crit Care. 2016;20(Suppl 2):94.
Schmidt M, Bailey M, Sheldrake J, Hodgson C, Aubron C, Rycus PT, et al. Predicting survival after extracorporeal membrane oxygenation for severe acute respiratory failure. The Respiratory Extracorporeal Membrane Oxygenation Survival Prediction (RESP) score. Am J Respir Crit Care Med. 2014;189(11):1374-82. DOI: https://doi.org/10.1164/rccm.201311-2023OC
Orsini J, Blaak C, Yeh A, Fonseca X, Helm T, Butala A, et al. Triage of Patients Consulted for ICU Admission During Times of ICU-Bed Shortage. J Clin Med Res. 2014;6(6):463-8. DOI: https://doi.org/10.14740/jocmr1939w
Dalia AA, Ortoleva J, Fiedler A, Villavicencio M, Shelton K, Cudemus GD. Extracorporeal Membrane Oxygenation Is a Team Sport: Institutional Survival Benefits of a Formalized ECMO Team. J Cardiothorac Vasc Anesth. 2019;33(4):902-7. DOI: https://doi.org/10.1053/j.jvca.2018.06.003
Fitzgerald DC, Darling EM, Cardona MF. Staffing, Equipment, Monitoring Considerations for Extracorporeal Membrane Oxygenation. Crit Care Clin. 2017;33(4):863-81. DOI: https://doi.org/10.1016/j.ccc.2017.06.008
Bjelic M, Kumar N, Gu Y, Chase K, Paic F, Gosev I. Cause of In-Hospital Death After Weaning from Venoarterial-Extracorporeal Membrane Oxygenation. J Intensive Care Med. 2022:8850666221086839. DOI: https://doi.org/10.1177/08850666221086839
Ayers B, Bjelic M, Kumar N, Wood K, Barrus B, Prasad S, et al. Long-term renal function after venoarterial extracorporeal membrane oxygenation. J Card Surg. 2021;36(3):815-20. DOI: https://doi.org/10.1111/jocs.15277
Amin F, Lombardi J, Alhussein M, Posada JD, Suszko A, Koo M, et al. Predicting Survival After VA-ECMO for Refractory Cardiogenic Shock: Validating the SAVE Score. CJC Open. 2021;3(1):71-81. DOI: https://doi.org/10.1016/j.cjco.2020.09.011
Appelt H, Philipp A, Mueller T, Foltan M, Lubnow M, Lunz D, et al. Factors associated with hemolysis during extracorporeal membrane oxygenation (ECMO)-Comparison of VA- versus VV ECMO. PLoS One. 2020;15(1):e0227793. DOI: https://doi.org/10.1371/journal.pone.0227793
Millar JE, Fanning JP, McDonald CI, McAuley DF, Fraser JF. The inflammatory response to extracorporeal membrane oxygenation (ECMO): a review of the pathophysiology. Crit Care. 2016;20(1):387. DOI: https://doi.org/10.1186/s13054-016-1570-4
Blakeslee-Carter J, Shao C, LaGrone R, Gonzalez-Sigler I, Sutzko DC, Pearce B, et al. Vascular complications based on mode of extracorporeal membrane oxygenation. J Vasc Surg. 2022;75(6):2037-46.e2. DOI: https://doi.org/10.1016/j.jvs.2022.01.078
Malinowski D, Fournier Y, Horbach A, Frick M, Magliani M, Kalverkamp S, et al. Computational fluid dynamics analysis of endoluminal aortic perfusion. Perfusion. 2022:2676591221099809. DOI: https://doi.org/10.1177/02676591221099809
Galvagno SM, Jr., Pelekhaty S, Cornachione CR, Deatrick KB, Mazzeffi MA, Scalea TM, et al. Does Weight Matter? Outcomes in Adult Patients on Venovenous Extracorporeal Membrane Oxygenation When Stratified by Obesity Class. Anesth Analg. 2020;131(3):754-61. DOI: https://doi.org/10.1213/ANE.0000000000004454
Swol J, Buchwald D, Strauch JT, Schildhauer TA, Ull C. Effect of body mass index on the outcome of surgical patients receiving extracorporeal devices (VV ECMO, pECLA) for respiratory failure. Int J Artif Organs. 2017:0. DOI: https://doi.org/10.5301/ijao.5000572
Muller G, Flecher E, Lebreton G, Luyt C-E, Trouillet J-L, Bréchot N, et al. The ENCOURAGE mortality risk score and analysis of long-term outcomes after VA-ECMO for acute myocardial infarction with cardiogenic shock. Intensive Care Medicine. 2016;42(3):370-8. DOI: https://doi.org/10.1007/s00134-016-4223-9
Published
How to Cite
License
Copyright (c) 2023 Andrew S Jones, George Olverson IV, Wayne Wong, Rohun Bhagat, Clauden Louis

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- The Author retains copyright in the Work, where the term “Work” shall include all digital objects that may result in subsequent electronic publication or distribution.
- Upon acceptance of the Work, the author shall grant to the Publisher the right of first publication of the Work.
- The Author shall grant to the Publisher and its agents the nonexclusive perpetual right and license to publish, archive, and make accessible the Work in whole or in part in all forms of media now or hereafter known under a Creative Commons Attribution 4.0 International License or its equivalent, which, for the avoidance of doubt, allows others to copy, distribute, and transmit the Work under the following conditions:
- Attribution—other users must attribute the Work in the manner specified by the author as indicated on the journal Web site; with the understanding that the above condition can be waived with permission from the Author and that where the Work or any of its elements is in the public domain under applicable law, that status is in no way affected by the license.
- The Author is able to enter into separate, additional contractual arrangements for the nonexclusive distribution of the journal's published version of the Work (e.g., post it to an institutional repository or publish it in a book), as long as there is provided in the document an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post online a prepublication manuscript (but not the Publisher’s final formatted PDF version of the Work) in institutional repositories or on their Websites prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. Any such posting made before acceptance and publication of the Work shall be updated upon publication to include a reference to the Publisher-assigned DOI (Digital Object Identifier) and a link to the online abstract for the final published Work in the Journal.
- Upon Publisher’s request, the Author agrees to furnish promptly to Publisher, at the Author’s own expense, written evidence of the permissions, licenses, and consents for use of third-party material included within the Work, except as determined by Publisher to be covered by the principles of Fair Use.
- The Author represents and warrants that:
- the Work is the Author’s original work;
- the Author has not transferred, and will not transfer, exclusive rights in the Work to any third party;
- the Work is not pending review or under consideration by another publisher;
- the Work has not previously been published;
- the Work contains no misrepresentation or infringement of the Work or property of other authors or third parties; and
- the Work contains no libel, invasion of privacy, or other unlawful matter.
- The Author agrees to indemnify and hold Publisher harmless from the Author’s breach of the representations and warranties contained in Paragraph 6 above, as well as any claim or proceeding relating to Publisher’s use and publication of any content contained in the Work, including third-party content.
Enforcement of copyright
The IJMS takes the protection of copyright very seriously.
If the IJMS discovers that you have used its copyright materials in contravention of the license above, the IJMS may bring legal proceedings against you seeking reparation and an injunction to stop you using those materials. You could also be ordered to pay legal costs.
If you become aware of any use of the IJMS' copyright materials that contravenes or may contravene the license above, please report this by email to contact@ijms.org
Infringing material
If you become aware of any material on the website that you believe infringes your or any other person's copyright, please report this by email to contact@ijms.org







