Effects of the COVID-19 Pandemic on Physical Activity in Children: A Systematic Review
DOI:
https://doi.org/10.5195/ijms.2024.1716Keywords:
COVID-19, Exercise, Children, Extended Lockdowns, Physical Activity, Systematic Review, Pandemic, Database Search, PRISMA, Unstructured Play, Virtual PA, Increased PA, Younger Children, Policies, Health Benefits, Immune system, Heart Diseases, Chronic Conditions, Type 2 Diabetes, ObesityAbstract
Background: Extended lockdowns established to minimize the spread of COVID-19, may have affected physical activity (PA). The objective of this systematic review was to report how PA of children was impacted by the COVID-19 pandemic.
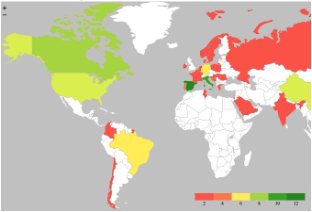
Methods: A database search of CINAHOL, Embase, MEDLINE, PsycInfo, and Web of Science was conducted on 03/29/2021 in accordance with Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines. Studies were included if they reported a measure of PA for children ≤18 years and were published in English in a peer-reviewed journal. The search generated 673 unique citations. After applying the criteria above, 69 articles were included. The quality of the included articles was assessed using the NIH NHLBI Study Quality Assessment Toolbox.
Results: Unstructured play, walking, and virtual PA (e.g., YouTube, online classes) were the most frequently reported modes of PA during the COVID-19 pandemic. The PA of children decreased among 89% of articles that reported changes in PA (e.g., frequency, intensity, duration, or the percentage of children who met PA recommendations) of children during the COVID-19 pandemic. Increased PA was reported more often among younger children, boys, children who lived with other children, and children with more outdoor space.
Conclusion: Globally, PA of children decreased during the COVID-19 pandemic. Further work is needed to develop policies to support global PA increases. Limitations of this review include the use of online surveys which are limited by participants ability to recall PA behaviors and access to online resources.
References
Rundle AG, Park Y, Herbstman JB, Kinsey EW, Wang YC. COVID-19-Related School Closings and Risk of Weight Gain Among Children. Obesity (Silver Spring). 2020;28(6):1008-1009.
Coronavirus disease 2019 (COVID-19): Situation Report. World Health Organization. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports
Nicola M, Alsafi Z, Sohrabi C, et al. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int J Surg. 2020;78:185-193.
Control CfD, Prevention. Low level lead exposure harms children: a renewed call for primary prevention. US Department of Health & Human Services, Centers for Disease Control and Prevention; 2012.
Foster C, Moore JB, Singletary CR, Skelton JA. Physical activity and family-based obesity treatment: a review of expert recommendations on physical activity in youth. Clinical Obesity. 2018;8(1):68-79.
Thivel D, Tremblay A, Genin PM, Panahi S, Rivière D, Duclos M. Physical Activity, Inactivity, and Sedentary Behaviors: Definitions and Implications in Occupational Health. Front Public Health. 2018;6:288-288.
Physical activity. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/physical-activity
Chaput J-P, Willumsen J, Bull F, et al. 2020 WHO guidelines on physical activity and sedentary behaviour for children and adolescents aged 5-17 years: summary of the evidence. The international journal of behavioral nutrition and physical activity. 2020;17(1):141-141.
Janssen I, Leblanc AG. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act. 2010;7:40.
Poitras VJ, Gray CE, Borghese MM, et al. Systematic review of the relationships between objectively measured physical activity and health indicators in school-aged children and youth. Appl Physiol Nutr Metab. 2016;41(6 Suppl 3).
Patterson R, McNamara E, Tainio M, et al. Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: a systematic review and dose response meta-analysis. Eur J Epidemiol. 2018;33(9):811-829.
Guthold R, Stevens GA, Riley LM, Bull FC. Global trends in insufficient physical activity among adolescents: a pooled analysis of 298 population-based surveys with 1.6 million participants. The Lancet Child & Adolescent Health. 2020;4(1):23-35.
Brazendale K, Beets MW, Weaver RG, et al. Understanding differences between summer vs. school obesogenic behaviors of children: the structured days hypothesis. International Journal of Behavioral Nutrition and Physical Activity. 2017;14(1):100.
Franckle R, Adler R, Davison K. Accelerated weight gain among children during summer versus school year and related racial/ethnic disparities: a systematic review. Prev Chronic Dis. 2014;11.
Siebach MK, Piedimonte G, Ley SH. COVID-19 in childhood: Transmission, clinical presentation, complications and risk factors. Pediatr Pulmonol. 2021;56(6):1342-1356.
Dhochak N, Singhal T, Kabra SK, Lodha R. Pathophysiology of COVID-19: Why Children Fare Better than Adults? Indian J Pediatr. 2020;87(7):537-546.
Okuyama J, Seto S, Fukuda Y, et al. Mental Health and Physical Activity among Children and Adolescents during the COVID-19 Pandemic. The Tohoku Journal of Experimental Medicine. 2021;253(3):203-215.
Ghosh R, Dubey MJ, Chatterjee S, Dubey S. Impact of COVID-19 on children: special focus on the psychosocial aspect. Minerva Pediatr. 2020;72(3):226-235.
Shrestha R, Copenhaver M. Long-Term Effects of Childhood Risk Factors on Cardiovascular Health During Adulthood. Clin Med Rev Vasc Health. 2015;7:1-5.
Kallio P, Pahkala K, Heinonen OJ, et al. Physical inactivity from youth to adulthood and adult cardiometabolic risk profile. Prev Med. 2021;145:106433.
Ruegsegger GN, Booth FW. Health Benefits of Exercise. Cold Spring Harb Perspect Med. 2018;8(7).
Lavie CJ, Ozemek C, Carbone S, Katzmarzyk PT, Blair SN. Sedentary Behavior, Exercise, and Cardiovascular Health. Circ Res. 2019;124(5):799-815.
Booth FW, Roberts CK, Laye MJ. Lack of exercise is a major cause of chronic diseases. Compr Physiol. 2012;2(2):1143-211.
Nieman DC, Wentz LM. The compelling link between physical activity and the body's defense system. J Sport Health Sci. 2019;8(3):201-217.
Nieman DC, Pence BD. Exercise immunology: Future directions. J Sport Health Sci. 2020;9(5):432-445.
Sallis R, Young DR, Tartof SY, et al. Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients. Br J Sports Med. 2021.
Williams N, Radia T, Harman K, Agrawal P, Cook J, Gupta A. COVID-19 Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in children and adolescents: a systematic review of critically unwell children and the association with underlying comorbidities. Eur J Pediatr. 2021;180(3):689-697.
Fernandes DM, Oliveira CR, Guerguis S, et al. Severe Acute Respiratory Syndrome Coronavirus 2 Clinical Syndromes and Predictors of Disease Severity in Hospitalized Children and Youth. J Pediatr. 2021;230:23-31.e10.
Gao YD, Ding M, Dong X, et al. Risk factors for severe and critically ill COVID-19 patients: A review. Allergy. 2021;76(2):428-455.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Bmj. 2021;372.
Yomoda K, Kurita S. Influence of social distancing during the COVID-19 pandemic on physical activity in children: A scoping review of the literature. J Exerc Sci Fit. 2021;19(3):195-203.
Quality assessment tool for observational cohort and cross-sectional studies. National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/node/80102
Alonso-Martinez AM, Ramirez-Velez R, Garcia-Alonso Y, Izquierdo M, Garcia-Hermoso A. Physical Activity, Sedentary Behavior, Sleep and Self-Regulation in Spanish Preschoolers during the COVID-19 Lockdown. International Journal of Environmental Research & Public Health. 2021;18(2):15.
Androutsos O, Perperidi M, Georgiou C, Chouliaras G. Lifestyle changes and determinants of children’s and adolescents’ body weight increase during the first COVID-19 lockdown in Greece: The COV-EAT study. Nutrients. 2021;13(3):1-11.
Cachon-Zagalaz J, Zagalaz-Sanchez ML, Arufe-Giraldez V, Sanmiguel-Rodriguez A, Gonzalez-Valero G. Physical Activity and Daily Routine among Children Aged 0-12 during the COVID-19 Pandemic in Spain. International Journal of Environmental Research & Public Health. 2021;18(2):15.
Chambonniere C, Lambert C, Fearnbach N, et al. Effect of the COVID-19 lockdown on physical activity and sedentary behaviors in French children and adolescents: New results from the ONAPS national survey. European Journal of Integrative Medicine. 2021;43:101308.
Delisle Nystrom C, Alexandrou C, Henstrom M, et al. International Study of Movement Behaviors in the Early Years (SUNRISE): Results from SUNRISE Sweden's Pilot and COVID-19 Study. International Journal of Environmental Research & Public Health. 2020;17(22):16.
Gilic B, Ostojic L, Corluka M, Volaric T, Sekulic D. Contextualizing Parental/Familial Influence on Physical Activity in Adolescents before and during COVID-19 Pandemic: A Prospective Analysis. Children. 2020;7(9):03.
Gilic B, Zenic N, Separovic V, Jurcev Savicevic A, Sekulic D. Evidencing the influence of pre-pandemic sports participation and substance misuse on physical activity during the COVID-19 lockdown: a prospective analysis among older adolescents. International Journal of Occupational Medicine & Environmental Health. 2021;22:22.
Sekulic D, Blazevic M, Gilic B, Kvesic I, Zenic N. Prospective Analysis of Levels and Correlates of Physical Activity during COVID-19 Pandemic and Imposed Rules of Social Distancing; Gender Specific Study among Adolescents from Southern Croatia. Sustainability. 2020;12(10)4072.
Zenic N, Taiar R, Gilic B, et al. Levels and Changes of Physical Activity in Adolescents during the COVID-19 Pandemic: Contextualizing Urban vs. Rural Living Environment. Applied Sciences-Basel. 2020;10(11)3997.
Francisco R, Pedro M, Delvecchio E, et al. Psychological Symptoms and Behavioral Changes in Children and Adolescents During the Early Phase of COVID-19 Quarantine in Three European Countries. Frontiers in psychiatry Frontiers Research Foundation. 2020;11:570164.
Hommes F, van Loon W, Thielecke M, et al. Sars-cov-2 infection, risk perception, behaviour and preventive measures at schools in berlin, germany, during the early post-lockdown phase: A cross-sectional study. International Journal of Environmental Research and Public Health. 2021;18(5):1-12.
Konstantinou C, Andrianou XD, Constantinou A, et al. Exposome changes in primary school children following the wide population non-pharmacological interventions implemented due to COVID-19 in Cyprus: A national survey. EClinicalMedicine. 2021;32:100721.
Kovacs Va Md P, Starc GP, Brandes MP, et al. Physical activity, screen time and the COVID-19 school closures in Europe - an observational study in 10 countries. European Journal of Sport Science EJSS: Official Journal of the European College of Sport Science. 2021:1-26.
Lopez-Bueno R, Calatayud J, Andersen LL, et al. Cardiorespiratory fitness in adolescents before and after the COVID-19 confinement: a prospective cohort study. Eur J Pediatr. 2021;17:17.
Lopez-Bueno R, Lopez-Sanchez GF, Casajus JA, et al. Health-Related Behaviors Among School-Aged Children and Adolescents During the Spanish Covid-19 Confinement. Frontiers in Pediatrics. 2020;8:573.
Medrano M, Cadenas-Sanchez C, Oses M, Arenaza L, Amasene M, Labayen I. Changes in lifestyle behaviours during the COVID-19 confinement in Spanish children: A longitudinal analysis from the MUGI project. Pediatric Obesity. 2021;16(4).
Lopez-Gil JF, Tremblay MS, Brazo-Sayavera J. Changes in Healthy Behaviors and Meeting 24-h Movement Guidelines in Spanish and Brazilian Preschoolers, Children and Adolescents during the COVID-19 Lockdown. Children. 2021;8(2):26.
Morgul E, Kallitsoglou A, Essau CA. Psychological effects of the COVID-19 lockdown on children and families in the UK. Revista de Psicologia Clinica con Ninos y Adolescentes. 2020;7(3):42-48.
Poulain T, Meigen C, Sobek C, et al. Loss of childcare and classroom teaching during the Covid-19-related lockdown in spring 2020: A longitudinal study on consequences on leisure behavior and schoolwork at home. PLoS ONE. 2021;16(3).
Ng K, Cooper J, McHale F, Clifford J, Woods C. Barriers and facilitators to changes in adolescent physical activity during COVID-19. BMJ Open Sport & Exercise Medicine. 2020;6(1).
Orgiles M, Morales A, Delvecchio E, Mazzeschi C, Espada JP. Immediate Psychological Effects of the COVID-19 Quarantine in Youth From Italy and Spain. Frontiers in Psychology. 2020;11:579038.
Pietrobelli A, Pecoraro L, Ferruzzi A, et al. Effects of COVID-19 Lockdown on Lifestyle Behaviors in Children with Obesity Living in Verona, Italy: A Longitudinal Study. Obesity. 2020;28(8):1382-1385.
Pombo A, Luz C, Rodrigues LP, Ferreira C, Cordovil R. Correlates of children's physical activity during the COVID-19 confinement in Portugal. Public Health. 2020;189:14-19.
Predieri B, Leo F, Candia F, et al. Glycemic Control Improvement in Italian Children and Adolescents With Type 1 Diabetes Followed Through Telemedicine During Lockdown Due to the COVID-19 Pandemic. Frontiers in Endocrinology. 2020;11:595735.
Roe A, Blikstad-Balas M, Dalland CP. The Impact of COVID-19 and Homeschooling on Students' Engagement With Physical Activity. Frontiers in Sports & Active Living. 2020;2:589227.
Ruiz-Roso MB, de Carvalho Padilha P, Matilla-Escalante DC, et al. Changes of Physical Activity and Ultra-Processed Food Consumption in Adolescents from Different Countries during Covid-19 Pandemic: An Observational Study. Nutrients. 2020;12(8):30.
Schmidt SCE, Anedda B, Burchartz A, et al. Physical activity and screen time of children and adolescents before and during the COVID-19 lockdown in Germany: a natural experiment. Scientific Reports. 2020;10(1):21780.
Schmidt T, Pawlowski CS. Physical Activity in Crisis: The Impact of COVID-19 on Danes' Physical Activity Behavior. Frontiers in Sports & Active Living. 2020;2:610255.
Salzano G, Passanisi S, Pira F, et al. Quarantine due to the COVID-19 pandemic from the perspective of adolescents: the crucial role of technology. Italian Journal of Pediatrics. 2021;47(1):40.
Ten Velde G, Lubrecht J, Arayess L, et al. Physical activity behaviour and screen time in Dutch children during the COVID-19 pandemic: Pre-, during- and post-school closures. Pediatric Obesity. 2021.
Theis N, Campbell N, De Leeuw J, Owen M, Schenke KC. The effects of COVID-19 restrictions on physical activity and mental health of children and young adults with physical and/or intellectual disabilities. Disability & Health Journal. 2021:101064.
Tornaghi M, Lovecchio N, Vandoni M, Chirico A, Codella R. Physical activity levels across COVID-19 outbreak in youngsters of Northwestern Lombardy. Journal of Sports Medicine & Physical Fitness. 2020;03:03.
Wunsch K, Nigg C, Niessner C, et al. The Impact of COVID-19 on the Interrelation of Physical Activity, Screen Time and Health-Related Quality of Life in Children and Adolescents in Germany: Results of the Motorik-Modul Study. Children. 2021;8(2):02.
Zorcec T, Jakovska T, Micevska V, Boskovska K, Cholakovska VC. Pandemic with COVID-19 and Families with Children with Chronic Respiratory Diseases. Prilozi Makedonska Akademija Na Naukite I Umetnostite Oddelenie Za Medicinski Nauki. 2020;41(2):95-101.
Carroll N, Sadowski A, Laila A, et al. The Impact of COVID-19 on Health Behavior, Stress, Financial and Food Security among Middle to High Income Canadian Families with Young Children. Nutrients. 2020;12(8):07.
Ellis WE, Dumas TM, Forbes LM. Physically isolated but socially connected: Psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Canadian Journal of Behavioural Science / Revue canadienne des sciences du comportement. 2020;52(3):177-187.
Guerrero MD, Vanderloo LM, Rhodes RE, Faulkner G, Moore SA, Tremblay MS. Canadian children's and youth's adherence to the 24-h movement guidelines during the COVID-19 pandemic: A decision tree analysis. Journal of Sport & Health Science. 2020;9(4):313-321.
Hemphill NM, Kuan MTY, Harris KC. Reduced Physical Activity During COVID-19 Pandemic in Children With Congenital Heart Disease. Canadian Journal of Cardiology. 2020;36(7):1130-1134.
McCormack GR, Doyle-Baker PK, Petersen JA, Ghoneim D. Parent anxiety and perceptions of their child's physical activity and sedentary behaviour during the COVID-19 pandemic in Canada. Preventive Medicine Reports. 2020;20:101275.
Mitra R, Moore SA, Gillespie M, et al. Healthy movement behaviours in children and youth during the COVID-19 pandemic: Exploring the role of the neighbourhood environment. Health & Place. 2020;65:102418.
Moore SA, Faulkner G, Rhodes RE, et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: a national survey. International Journal of Behavioral Nutrition & Physical Activity. 2020;17(1):85.
Bazett-Jones DM, Garcia MC, Taylor-Haas JA, et al. Impact of COVID-19 Social Distancing Restrictions on Training Habits, Injury, and Care Seeking Behavior in Youth Long-Distance Runners. Frontiers in Sports & Active Living. 2020;2:586141.
Dunton GF, Do B, Wang SD. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC Public Health. 2020;20(1):1351.
Garcia JM, Lawrence S, Brazendale K, Leahy N, Fukuda D. Brief report: The impact of the COVID-19 pandemic on health behaviors in adolescents with Autism Spectrum Disorder. Disability & Health Journal. 2020:101021.
McGuine TA, Biese KM, Petrovska L, et al. Mental Health, Physical Activity, and Quality of Life of US Adolescent Athletes During COVID-19-Related School Closures and Sport Cancellations: A Study of 13 000 Athletes. Journal of Athletic Training. 2020;08:08.
Pavlovic A, DeFina LF, Natale BL, et al. Keeping children healthy during and after COVID-19 pandemic: meeting youth physical activity needs. BMC Public Health. 2021;21(1):485.
Tulchin-Francis K, Stevens W, Jr., Gu X, et al. The impact of the coronavirus disease 2019 pandemic on physical activity in US children. Journal of Sport & Health Science. 2021;28:28.
de Matos DG, Aidar FJ, De Almeida PF, et al. The Impact of Measures Recommended by the Government to Limit the Spread of Coronavirus (COVID-19) on Physical Activity Levels, Quality of Life, and Mental Health of Brazilians. Sustainability. 2020;12(21)9072.
Sa C, Pombo A, Luz C, Rodrigues LP, Cordovil R. Covid-19 Social Isolation in Brazil: Effects on the Physical Activity Routine of Families with Children. Revista Paulista de Pediatria. 2020;39.
Siegle CBH, Pombo A, Luz C, Rodrigues LP, Cordovil R, Sa C. Influences of Family and Household Characteristics on Children's Level of Physical Activity during Social Distancing Due to Covid-19 in Brazil. Revista Paulista de Pediatria. 2020;39.
Aguilar-Farias N, Toledo-Vargas M, Miranda-Marquez S, et al. Sociodemographic Predictors of Changes in Physical Activity, Screen Time, and Sleep among Toddlers and Preschoolers in Chile during the COVID-19 Pandemic. International Journal of Environmental Research & Public Health. 2020;18(1):29.
Reece LJ, Owen K, Foley B, Rose C, Bellew B, Bauman A. Understanding the impact of COVID-19 on children's physical activity levels in NSW, Australia. Health Promotion Journal of Australia. 2020;17:17.
Cahal M, Amirav I, Diamant N, Be'er M, Besor O, Lavie M. Real-time effects of COVID-19 pandemic lockdown on pediatric respiratory patients. Pediatric Pulmonology. 2021;17:17.
Chaturvedi K, Vishwakarma DK, Singh N. COVID-19 and its impact on education, social life and mental health of students: A survey. Children & Youth Services Review. 2021;121:105866.
Ghanamah R, Eghbaria-Ghanamah H. Impact of covid-19 pandemic on behavioral and emotional aspects and daily routines of Arab israeli children. International Journal of Environmental Research and Public Health. 2021;18(6):1-19.
Masi A, Mendoza Diaz A, Tully L, et al. Impact of the COVID-19 pandemic on the well-being of children with neurodevelopmental disabilities and their parents. Journal of Paediatrics & Child Health. 2021;10:10.
Munasinghe S, Sperandei S, Freebairn L, et al. The Impact of Physical Distancing Policies During the COVID-19 Pandemic on Health and Well-Being Among Australian Adolescents. Journal of Adolescent Health. 2020;67(5):653-661.
Nathan A, George P, Ng M, et al. Impact of covid-19 restrictions on western Australian children’s physical activity and screen time. International Journal of Environmental Research and Public Health. 2021;18(5):1-13.
Parker K, Uddin R, Ridgers ND, et al. The Use of Digital Platforms for Adults' and Adolescents' Physical Activity During the COVID-19 Pandemic (Our Life at Home): Survey Study. Journal of Medical Internet Research. 2021;23(2).
Sciberras E, Patel P, Stokes MA, et al. Physical Health, Media Use, and Mental Health in Children and Adolescents With ADHD During the COVID-19 Pandemic in Australia. Journal of Attention Disorders. 2020:1087054720978549.
Zhao Y, Guo Y, Xiao Y, et al. The Effects of Online Homeschooling on Children, Parents, and Teachers of Grades 1-9 During the COVID-19 Pandemic. Medical Science Monitor. 2020;26.
Adolescent Health. World Health Organization. https://www.who.int/health-topics/adolescent-health#tab=tab_1
Wu X, Luo S, Zheng X, et al. Glycemic control in children and teenagers with type 1 diabetes around lockdown for COVID-19: A continuous glucose monitoring-based observational study. Journal of Diabetes Investigation. 2021;04:04.
Zhang X, Zhu W, Kang S, Qiu L, Lu Z, Sun Y. Association between Physical Activity and Mood States of Children and Adolescents in Social Isolation during the COVID-19 Epidemic. International Journal of Environmental Research & Public Health. 2020;17(20):21.
Abid R, Ammar A, Maaloul R, Souissi N, Hammouda O. Effect of COVID-19-related home confinement on sleep quality, screen time and physical activity in tunisian boys and girls: A survey. International Journal of Environmental Research and Public Health. 2021;18(6):1-12.
Shinomiya Y, Yoshizaki A, Murata E, Fujisawa TX, Taniike M, Mohri I. Sleep and the General Behavior of Infants and Parents during the Closure of Schools as a Result of the COVID-19 Pandemic: Comparison with 2019 Data. Children. 2021;8(2):22.
Xiang M, Zhang Z, Kuwahara K. Impact of COVID-19 pandemic on children and adolescents' lifestyle behavior larger than expected. Progress in Cardiovascular Diseases. 2020;63(4):531-532.
Yang S, Guo B, Ao L, et al. Obesity and activity patterns before and during COVID-19 lockdown among youths in China. Clinical Obesity. 2020;10(6).
Elnaggar RK, Alqahtani BA, Mahmoud WS, Elfakharany MS. Physical Activity in Adolescents During the Social Distancing Policies of the COVID-19 Pandemic. Asia-Pacific Journal of Public Health. 2020;32(8):491-494.
Jia P, Zhang L, Yu W, et al. Impact of COVID-19 lockdown on activity patterns and weight status among youths in China: the COVID-19 Impact on Lifestyle Change Survey (COINLICS). International Journal of Obesity. 2021;45(3):695-699.
Prince SA, Butler GP, Rao DP, Thompson W. Evidence synthesis - Where are children and adults physically active and sedentary? - a rapid review of location-based studies. Health Promot Chronic Dis Prev Can. 2019;39(3):67-103.
Kelso A, Reimers AK, Abu-Omar K, et al. Locations of Physical Activity: Where Are Children, Adolescents, and Adults Physically Active? A Systematic Review. Int J Environ Res Public Health. 2021;18(3).
Weaver RG, Beets MW, Perry M, et al. Changes in children's sleep and physical activity during a 1-week versus a 3-week break from school: a natural experiment. Sleep. 2019;42(1).
Marzi I, Demetriou Y, Reimers AK. Social and physical environmental correlates of independent mobility in children: a systematic review taking sex/gender differences into account. Int J Health Geogr. 2018;17(1):24.
Steene-Johannessen J, Hansen BH, Dalene KE, et al. Variations in accelerometry measured physical activity and sedentary time across Europe - harmonized analyses of 47,497 children and adolescents. Int J Behav Nutr Phys Act. 2020;17(1):38.
D'Angelo H, Fowler SL, Nebeling LC, Oh AY. Adolescent Physical Activity: Moderation of Individual Factors by Neighborhood Environment. Am J Prev Med. 2017;52(6):888-894.
Alharbi M. Influence of individual and family factors on physical activity among Saudi girls: a cross-sectional study. Ann Saudi Med. 2019;39(1):13-21.
Lu C, Stolk RP, Sauer PJ, et al. Factors of physical activity among Chinese children and adolescents: a systematic review. Int J Behav Nutr Phys Act. 2017;14(1):36.
Reimers AK, Schmidt SCE, Demetriou Y, Marzi I, Woll A. Parental and peer support and modelling in relation to domain-specific physical activity participation in boys and girls from Germany. PLoS One. 2019;14(10).
Best K, Ball K, Zarnowiecki D, Stanley R, Dollman J. In Search of Consistent Predictors of Children's Physical Activity. Int J Environ Res Public Health. 2017;14(10).
Dishman RK, McIver KL, Dowda M, Saunders RP, Pate RR. Self-efficacy, beliefs, and goals: Moderation of declining physical activity during adolescence. Health Psychol. 2019;38(6):483-493.
Burns RD, Bai Y, Fu Y, Pfledderer CD, Brusseau TA. Parent Engagement and Support, Physical Activity, and Academic Performance (PESPAAP): A Proposed Theoretical Model. Int J Environ Res Public Health. 2019;16(23).
Khan SR, Uddin R, Mandic S, Khan A. Parental and Peer Support are Associated with Physical Activity in Adolescents: Evidence from 74 Countries. Int J Environ Res Public Health. 2020;17(12).
Haidar A, Ranjit N, Archer N, Hoelscher DM. Parental and peer social support is associated with healthier physical activity behaviors in adolescents: a cross-sectional analysis of Texas School Physical Activity and Nutrition (TX SPAN) data. BMC Public Health. 2019;19(1):640.
Cooper AR, Goodman A, Page AS, et al. Objectively measured physical activity and sedentary time in youth: the International children's accelerometry database (ICAD). The international journal of behavioral nutrition and physical activity. 2015;12:113-113.
Craggs C, Corder K, van Sluijs EM, Griffin SJ. Determinants of change in physical activity in children and adolescents: a systematic review. Am J Prev Med. 2011;40(6):645-58.
Hu D, Zhou S, Crowley-McHattan ZJ, Liu Z. Factors That Influence Participation in Physical Activity in School-Aged Children and Adolescents: A Systematic Review from the Social Ecological Model Perspective. International journal of environmental research and public health. 2021;18(6):3147.
Corder K, Sharp SJ, Atkin AJ, et al. Change in objectively measured physical activity during the transition to adolescence. Br J Sports Med. 2015;49(11):730-6.
Pate RR, Sallis JF, Ward DS, et al. Age-related changes in types and contexts of physical activity in middle school girls. Am J Prev Med. 2010;39(5):433-9.
Rhodes RE, Guerrero MD, Vanderloo LM, et al. Development of a consensus statement on the role of the family in the physical activity, sedentary, and sleep behaviours of children and youth. Int J Behav Nutr Phys Act. 2020;17(1):74.
Edwards MJ, Jago R, Sebire SJ, Kesten JM, Pool L, Thompson JL. The influence of friends and siblings on the physical activity and screen viewing behaviours of children aged 5-6 years: a qualitative analysis of parent interviews. BMJ Open. 2015;5(5).
Loebach J, Sanches M, Jaffe J, Elton-Marshall T. Paving the Way for Outdoor Play: Examining Socio-Environmental Barriers to Community-Based Outdoor Play. Int J Environ Res Public Health. 2021;18(7).
Euler R, Jimenez EY, Sanders S, et al. Rural-Urban Differences in Baseline Dietary Intake and Physical Activity Levels of Adolescents. Prev Chronic Dis. 2019;16.
Rivera-Ochoa M, Brazo-Sayavera J, Vizmanos-Lamotte B, et al. Health-Related Factors in Rural and Urban Mexican Adolescents from the State of Jalisco: The HELENA-MEX Study. Int J Environ Res Public Health. 2020;17(23).
Adebusoye B, Phalkey R, Leonardi-Bee J, Chattopadhyay K. Association of the built environment with physical activity in children and adolescents in Africa: a systematic review protocol. JBI Evidence Synthesis. 2020;18(3):553-563.
Gray C, Gibbons R, Larouche R, et al. What Is the Relationship between Outdoor Time and Physical Activity, Sedentary Behaviour, and Physical Fitness in Children? A Systematic Review. Int J Environ Res Public Health. 2015;12(6):6455-74.
Larouche R, Garriguet D, Gunnell KE, Goldfield GS, Tremblay MS. Outdoor time, physical activity, sedentary time, and health indicators at ages 7 to 14: 2012/2013 Canadian Health Measures Survey. Health Rep. 2016;27(9):3-13.
Lindsay AC, Greaney ML, Wallington SF, Mesa T, Salas CF. A review of early influences on physical activity and sedentary behaviors of preschool-age children in high-income countries. Journal for Specialists in Pediatric Nursing. 2017;22(3).
Christiana RW, Bouldin ED, Battista RA. Active living environments mediate rural and non-rural differences in physical activity, active transportation, and screen time among adolescents. Prev Med Rep. 2021;23:101422-101422.
Okazaki K, Suzuki K, Sakamoto Y, Sasaki K. Physical activity and sedentary behavior among children and adolescents living in an area affected by the 2011 Great East Japan earthquake and tsunami for 3 years. Prev Med Rep. 2015;2:720-724
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2023 Alex Ramirez, Ashley B. Rapp, Sara Santarossa

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- The Author retains copyright in the Work, where the term “Work” shall include all digital objects that may result in subsequent electronic publication or distribution.
- Upon acceptance of the Work, the author shall grant to the Publisher the right of first publication of the Work.
- The Author shall grant to the Publisher and its agents the nonexclusive perpetual right and license to publish, archive, and make accessible the Work in whole or in part in all forms of media now or hereafter known under a Creative Commons Attribution 4.0 International License or its equivalent, which, for the avoidance of doubt, allows others to copy, distribute, and transmit the Work under the following conditions:
- Attribution—other users must attribute the Work in the manner specified by the author as indicated on the journal Web site; with the understanding that the above condition can be waived with permission from the Author and that where the Work or any of its elements is in the public domain under applicable law, that status is in no way affected by the license.
- The Author is able to enter into separate, additional contractual arrangements for the nonexclusive distribution of the journal's published version of the Work (e.g., post it to an institutional repository or publish it in a book), as long as there is provided in the document an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post online a prepublication manuscript (but not the Publisher’s final formatted PDF version of the Work) in institutional repositories or on their Websites prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. Any such posting made before acceptance and publication of the Work shall be updated upon publication to include a reference to the Publisher-assigned DOI (Digital Object Identifier) and a link to the online abstract for the final published Work in the Journal.
- Upon Publisher’s request, the Author agrees to furnish promptly to Publisher, at the Author’s own expense, written evidence of the permissions, licenses, and consents for use of third-party material included within the Work, except as determined by Publisher to be covered by the principles of Fair Use.
- The Author represents and warrants that:
- the Work is the Author’s original work;
- the Author has not transferred, and will not transfer, exclusive rights in the Work to any third party;
- the Work is not pending review or under consideration by another publisher;
- the Work has not previously been published;
- the Work contains no misrepresentation or infringement of the Work or property of other authors or third parties; and
- the Work contains no libel, invasion of privacy, or other unlawful matter.
- The Author agrees to indemnify and hold Publisher harmless from the Author’s breach of the representations and warranties contained in Paragraph 6 above, as well as any claim or proceeding relating to Publisher’s use and publication of any content contained in the Work, including third-party content.
Enforcement of copyright
The IJMS takes the protection of copyright very seriously.
If the IJMS discovers that you have used its copyright materials in contravention of the license above, the IJMS may bring legal proceedings against you seeking reparation and an injunction to stop you using those materials. You could also be ordered to pay legal costs.
If you become aware of any use of the IJMS' copyright materials that contravenes or may contravene the license above, please report this by email to contact@ijms.org
Infringing material
If you become aware of any material on the website that you believe infringes your or any other person's copyright, please report this by email to contact@ijms.org







