Prevalence of Generalized Anxiety Disorder and Associated Risk Factors Among Medical Students in Sudan: A Cross-Sectional Study at Omdurman Islamic University
DOI:
https://doi.org/10.5195/ijms.2024.2095Keywords:
Generalized Anxiety Disorder, Medical Students, Prevalence, Risk Factors, Cross-Sectional Studies, Academic Performance, Mental Health, Socioeconomic Factors, Psychological Stress, Quality of Life, Sudan, Gender Differences, Chronic Disease Care, Exercise, Smoking, Stress, Psychological, Anxiety Disorders, Health Surveys, Educational Measurement, Drug Resistance, microbial; antimicrobial stewardship; health knowledge, attitudes, practices; COVID 19Abstract
Background: Generalized Anxiety Disorder (GAD) is a mental illness that significantly affects various domains of daily functioning. Limited research has been conducted on GAD among medical students in Sudan, particularly during the socio-political and economic crises. This study aimed to assess the prevalence of GAD, identify risk factors, and evaluate its impact on academic performance and daily activities among Sudanese medical students.
Methods: A cross-sectional study was conducted among undergraduate medical students at Omdurman Islamic University. Data were collected using a self-administered online questionnaire via Google Forms, consisting of two parts: socio-demographic information and the Generalized Anxiety Disorder Questionnaire (GAD-7), a validated tool for screening and measuring the severity of GAD.
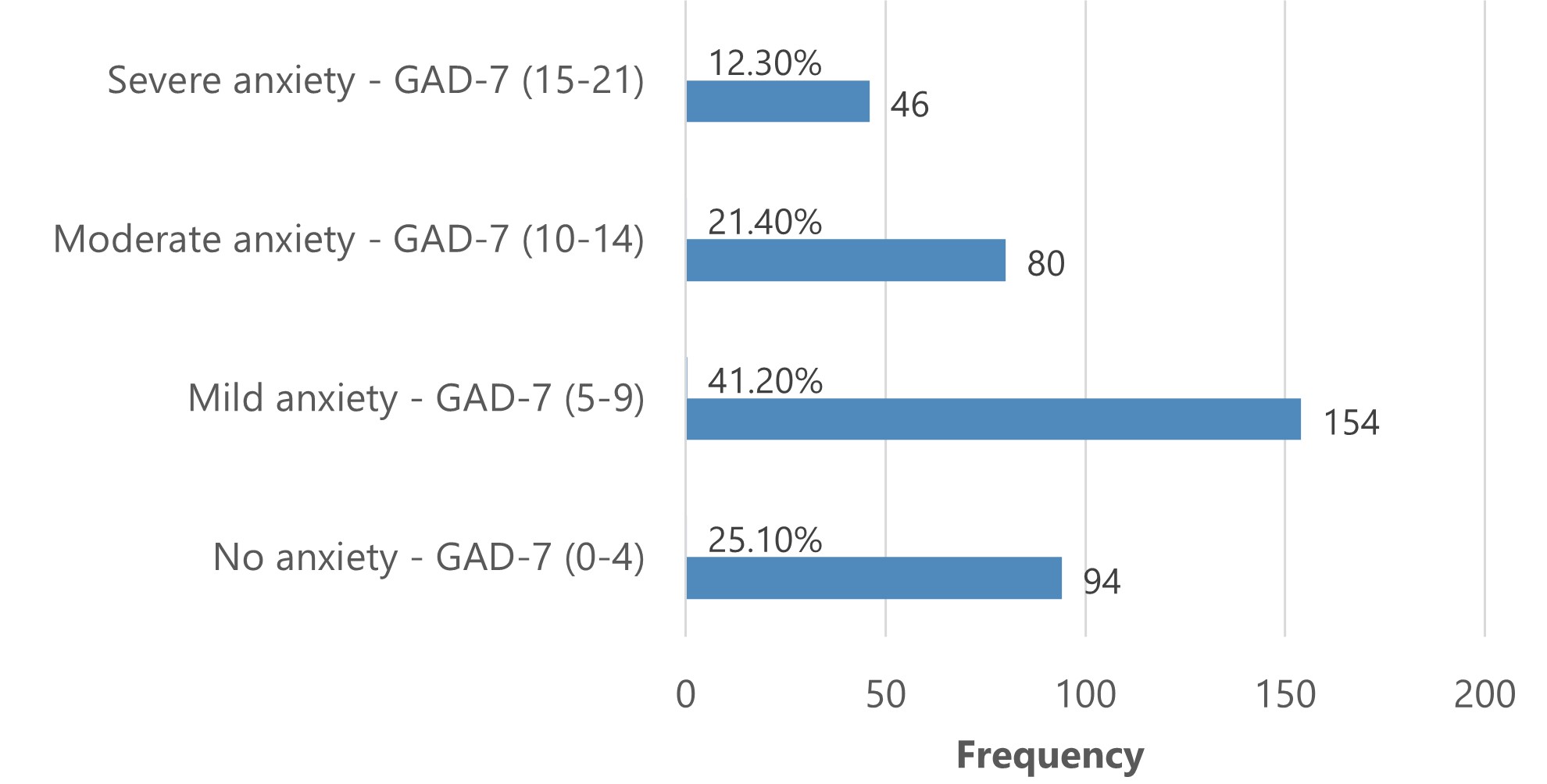
Results: A total of 374 medical students participated, with 64.7% being female. The GAD-7 scores were high (above 9), suggesting GAD among 33.7% of participants, with severity levels of 41.2% for mild anxiety, 21.4% for moderate anxiety, and 12.3% for severe anxiety. Comparison of means showed significant associations between GAD and female students (p<0.001) and students with chronic diseases (p=0.034). GAD significantly impacted daily activities (p<0.001). Multiple logistic regression analysis found that students in the final year had significantly higher GAD-7 scores (Adjusted Odds Ratio=4.25, 95% Confidence Interval=1.27-14.22).
Conclusions: The higher scores on the GAD-7 measure among Sudanese medical students are concerning. This emphasizes the urgent need to raise awareness, normalize mental health discussions, and provide accessible counseling services tailored to the students' needs.
References
World Health Organization. WHO highlights urgent need to transform mental health and mental health care. Available from: https://www.who.int/news/item/17-06-2022-who-highlights-urgent-need-to-transform-mental-health-and-mental-health-care. Last updated June 17, 2022; cited Feb 5, 2024.
Centers for Disease Control and Prevention. Symptoms of Generalized Anxiety Disorder Among Adults: United States, 2019; Available from: https://www.cdc.gov/nchs/products/index.htm. Last updated Sep 2020; cited Feb 4, 2024
Mishra AK, Varma AR. A Comprehensive Review of the Generalized Anxiety Disorder. Cureus. 2023;15(9):e46115.
National Institute of Mental Health (NIMH). Generalized Anxiety Disorder. Available from: https://www.nimh.nih.gov/health/statistics/generalized-anxiety-disorder; cited Feb 4, 2024
McLean CP, Asnaani A, Litz BT, Hofmann SG. Gender differences in anxiety disorders: Prevalence, course of illness, comorbidity and burden of illness. J Psychiatr Res. 2011;45(8):1027–35.
Bahrami F, Yousefi N. Females Are More Anxious Than Males: a Metacognitive Perspective. Iran J Psychiatry Behav Sci. 2011;5(2): 83-90.
Vesga-López O, Schneier F, Wang S, Heimberg R, Liu SM, Hasin DS, et al. Gender differences in Generalized Anxiety Disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). J Clin Psychiatry. 2008;69(10):1606-16.
Gottschalk M, Domschke K. Genetics of generalized anxiety disorder and related traits. Dialogues Clin Neurosci. 2017;19(2):159–68.
Huang CJ, Hsieh HM, Tu HP, Jiang HJ, Wang PW, Lin CH. Generalized anxiety disorder in type 2 diabetes mellitus: Prevalence and clinical characteristics. Brazilian Journal of Psychiatry. 2020;42(6):621–9.
Lavoie KL, Boudreau M, Plourde A, Campbell TS, Bacon SL. Association between generalized anxiety disorder and asthma morbidity. Psychosom Med. 2011;73(6):504–13.
Liao J, KJ, LF et al. A cross-sectional study on the Association of Anxiety and depression with the disease activity of systemic lupus erythematosus. BMC Psychiatry. 2022;22(1) 591.
Quek TTC, Tam WWS, Tran BX, Zhang M, Zhang Z, Ho CSH, et al. The global prevalence of anxiety among medical students: A meta-analysis. Int J Environ Res Public Health. 2019;16(15):2735.
Halperin SJ, Henderson MN, Prenner S, Grauer JN. Prevalence of Anxiety and Depression Among Medical Students During the Covid-19 Pandemic: A Cross-Sectional Study. J Med Educ Curric Dev. 2021;8:238212052199115.
Wali RM, Bagabas TM, Hassanein AA, Saad Alameri M, Fahad K, Ouqla A. The Prevalence and Risk Factors of Depression and Anxiety Disorders among Medical Students in King Saud Bin Abdulaziz University for Health Sciences, Jeddah 2019. Ann Med Health Sci Res. 2021;11:1-10.
Gabal HA , Wahdan MM, Gamal Eldin DA. Prevalence of anxiety, depression and stress among medical students, and associated factors. Egypt J Occup Med. 2022;46(1):55–74.
Barbosa-Camacho FJ, Romero-Limón OM, Ibarrola-Peña JC, Almanza-Mena YL, Pintor-Belmontes KJ, Sánchez-López VA, et al. Depression, anxiety, and academic performance in COVID-19: a cross-sectional study. BMC Psychiatry. 2022 Dec;22(1)434.
Jamil H, Alakkari M, Al-Mahini MS, Alsayid M, Al Jandali O. The Impact of Anxiety and Depression on Academic Performance: A Cross-Sectional Study among Medical Students in Syria. Avicenna J Med. 2022;12(03):111–9.
Gan GG, Hue YL. Anxiety, depression and quality of life of medical students in Malaysia. Med J Malaysia. 2019;74(1):57-61.
Wilmer MT, Anderson K, Reynolds M. Correlates of Quality of Life in Anxiety Disorders: Review of Recent Research. Curr Psychiatry Rep. 2021;23(11):77.
Mohamed OGN, Mohamed EGN, Ahmed R, Aburas L, Ali M, Hamdan HZ. Depression, Anxiety, and Stress among Sudanese Medical Students during the COVID-19 Lockdown Period. Open Access Maced J Med Sci. 2022;10(B):1365–71.
Mustafa SH, Mohammed EA, Makkawi ST, Mohammed YY. Mental Distress among Medical Students in Khartoum, Sudan 2022. Open J Psychiatr. 2022;12(04):345–58.
Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092-7.
Löwe B, Decker O, Müller S, Brähler E, Schellberg D, Herzog W, et al. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care. 2008;46(3):266-74.
Ibrahim D, Ahmed RM, Mohammad AZ, Ibrahim B, Mohammed T, Mohamed ME, et al. Prevalence and correlates of generalized anxiety disorder and perceived stress among Sudanese medical students. BMC Psychiatry. 2024;24(1):68.
Alatawi A, Alghamdi A, Albalwi A, Altayar M, Jalal M, Frah EAM. Prevalence of Generalized Anxiety Disorder (GAD) Among Saudi Medical Students and Associated Risk Factors. International Journal of Medical Research & Health Sciences. 2020; 5(9):1-9
Soltan MR, Soliman SS, Dawoud ME. A study of anxiety, depression and stress symptoms among Fayoum medical students during COVID-19 lockdown, Egypt. Egypt J Neurol Psychiatr Neurosurg. 2021;57(1):123.
Fawzy M, Hamed SA. Prevalence of psychological stress, depression and anxiety among medical students in Egypt. Psychiatry Res. 2017 ;255:186–94.
Jafri SAM, Zaidi E, Aamir IS, et al. Stress Level Comparison of Medical and Nonmedical Students: A Cross Sectional Study done at Various Professional Colleges in Karachi, Pakistan. Acta Psychopathologica. 2017;03(02).
Mohamed EY. Generalized anxiety disorder among saudi university medical students. Academic Journal of Health Sciences 2022;37(3):162-165.
Çimen İD, Alvur TM, Coşkun B, Şükür NEÖ. Mental health of Turkish medical students during the COVID-19 pandemic. Int J Soc Psychiatry. 2022;68(6):1253–62.
Abdel Wahed WY, Hassan SK. Prevalence and associated factors of stress, anxiety and depression among medical Fayoum University students. Alexandria Journal of Medicine. 2017;53(1):77–84.
Seeman M V. Psychopathology in Women and Men: Focus on Female Hormones. Am J Psychiatry. 1997;154(12):1641-7.
Altemus M. Sex differences in depression and anxiety disorders: Potential biological determinants. Horm Behav. 2006;50(4):534–8.
Backović D V, Živojinović JI, Maksimović J, Maksimović M. Gender differences in academic stress and burnout among medical students in final years of education. Psychiatr Danub. 2012;24(2):175-81.
Villwock JA, Sobin LB, Koester LA, Harris TM. Impostor syndrome and burnout among American medical students: a pilot study. Int J Med Educ. 2016;7:364–9.
Rice J, Rosario-Williams B, Williams F, West-Livingston L, Savage D, Wilensky JA, et al. Impostor syndrome among minority medical students who are underrepresented in medicine. J Natl Med Assoc. 2023;115(2):191–8.
Niemi PM, Vainiomäki PT. Medical students’ distress - Quality, continuity and gender differences during a six-year medical programme. Med Teach. 2006;28(2):136–41.
Dyrbye LN, Thomas MR, Shanafelt TD. Medical student distress: Causes, consequences, and proposed solutions. Mayo Clin Proc. 2005;80(12):1613–22.
von der Embse N, Jester D, Roy D, Post J. Test anxiety effects, predictors, and correlates: A 30-year meta-analytic review. J Affect Disord. 2018;227:483-493.
Teh CK, Ngo CW, Zulkifli RA binti, Vellasamy R, Suresh K. Depression, Anxiety and Stress among Undergraduate Students: A Cross Sectional Study. Open J Epidemiol. 2015;05(04):260–8.
Comer JS, Blanco C, Hasin DS, Liu SM, Grant BF, Turner JB, et al. Health-related quality of life across the anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). Journal of Clinical Psychiatry. 2011;72(1):43–50.
Mc Dowell CP, Carlin A, Capranica L, Dillon C, Harrington JM, Lakerveld J, et al. Associations of self-reported physical activity and anxiety symptoms and status among 7,874 Irish adults across harmonised datasets: A DEDIPAC-study. BMC Public Health. 2020 20;20(1).
Aylett E, Small N, Bower P. Exercise in the treatment of clinical anxiety in general practice - A systematic review and meta-analysis. BMC Health Serv Res. 2018 ;18(1):559.
Herring MP, Monroe DC, Gordon BR, Hallgren M, Campbell MJ. Acute Exercise Effects among Young Adults with Analogue Generalized Anxiety Disorder. Med Sci Sports Exerc. 2019;51(5):962–9.
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2024 Khalid Osman Mohamed, Ahmed ALemam Ahmed, ElShimaa Ammar Zaki, Sozan Mudather Soumit, Wamda Ahmed Allam, Asmaa Mohamed Mohamed

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- The Author retains copyright in the Work, where the term “Work” shall include all digital objects that may result in subsequent electronic publication or distribution.
- Upon acceptance of the Work, the author shall grant to the Publisher the right of first publication of the Work.
- The Author shall grant to the Publisher and its agents the nonexclusive perpetual right and license to publish, archive, and make accessible the Work in whole or in part in all forms of media now or hereafter known under a Creative Commons Attribution 4.0 International License or its equivalent, which, for the avoidance of doubt, allows others to copy, distribute, and transmit the Work under the following conditions:
- Attribution—other users must attribute the Work in the manner specified by the author as indicated on the journal Web site; with the understanding that the above condition can be waived with permission from the Author and that where the Work or any of its elements is in the public domain under applicable law, that status is in no way affected by the license.
- The Author is able to enter into separate, additional contractual arrangements for the nonexclusive distribution of the journal's published version of the Work (e.g., post it to an institutional repository or publish it in a book), as long as there is provided in the document an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post online a prepublication manuscript (but not the Publisher’s final formatted PDF version of the Work) in institutional repositories or on their Websites prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. Any such posting made before acceptance and publication of the Work shall be updated upon publication to include a reference to the Publisher-assigned DOI (Digital Object Identifier) and a link to the online abstract for the final published Work in the Journal.
- Upon Publisher’s request, the Author agrees to furnish promptly to Publisher, at the Author’s own expense, written evidence of the permissions, licenses, and consents for use of third-party material included within the Work, except as determined by Publisher to be covered by the principles of Fair Use.
- The Author represents and warrants that:
- the Work is the Author’s original work;
- the Author has not transferred, and will not transfer, exclusive rights in the Work to any third party;
- the Work is not pending review or under consideration by another publisher;
- the Work has not previously been published;
- the Work contains no misrepresentation or infringement of the Work or property of other authors or third parties; and
- the Work contains no libel, invasion of privacy, or other unlawful matter.
- The Author agrees to indemnify and hold Publisher harmless from the Author’s breach of the representations and warranties contained in Paragraph 6 above, as well as any claim or proceeding relating to Publisher’s use and publication of any content contained in the Work, including third-party content.
Enforcement of copyright
The IJMS takes the protection of copyright very seriously.
If the IJMS discovers that you have used its copyright materials in contravention of the license above, the IJMS may bring legal proceedings against you seeking reparation and an injunction to stop you using those materials. You could also be ordered to pay legal costs.
If you become aware of any use of the IJMS' copyright materials that contravenes or may contravene the license above, please report this by email to contact@ijms.org
Infringing material
If you become aware of any material on the website that you believe infringes your or any other person's copyright, please report this by email to contact@ijms.org







