Medical Students’ Stress Levels Are Correlated with Their Sleep Quality and Life Satisfaction
DOI:
https://doi.org/10.5195/ijms.2024.2239Keywords:
Medical Students , Stress, Psychological, Sleep Quality, Life Satisfaction, Cross-Sectional Studies, Anxiety, Cortisol, Blood Pressure, Heart rate, Saliva, Biological Markers, Gender Differences, Body Mass Index (BMI), Alcohol Drinking, Smoking, Caffeine, Sleep Disorders, Psychological Well-being, Academic Performance, Health SurveysAbstract
Background: Stress and sleep disturbances associated with low life satisfaction is frequently reported during medical education, intervening with the academic achievements and general well-being of medical students. We aimed to investigate the effects of stress levels on sleep quality (SQ) and life satisfaction (LS) of the students in Hacettepe University Medical Faculty (HUMF).
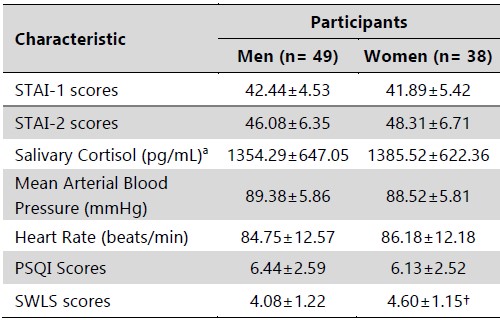
Methods: This cross-sectional study was conducted at HUMF between May and September 2022 after ethical approval. The participants (39 women and 48 men) completed a personal information form, State- Trait Anxiety Index (STAI)-I and II, Pittsburgh SQ Index (PSQI) and Satisfaction with Life Scale (SWLS). Their blood pressure, heart rate, and salivary cortisol levels were measured.
Results: The men and women were comparable for age, body mass index (BMI), stress parameters and PSQI scores, except the higher LS in women (P=0.045). Gender-based analysis revealed positively correlated BMI and STAI-I (r=0.357) and II (r=0.501) scores in women (P<0.05), and a similar but a weaker correlation for STAI-II scores in men (r=0.291) (P<0.05). The study group exhibited poor SQ (>5). The higher STAI-II scores, cortisol concentration and caffeine consumption were significantly associated with poorer SQ and LS in both genders, however, the state scores and alcohol consumption exhibited a significant relation in men, only. Higher scores for trait inventory and cortisol concentrations correlated negatively with LS in all participants.
Conclusion: Awareness, a proactive approach, and sufficient support can help the relieve and/or manage the stress of medical students and improve SQ and LS.
References
Shin DC, Johnson DM. Avowed happiness as an overall assessment of the quality of life. Social Indicators Research. 1978;5(1-4):475-92.
Diener E, Emmons RA, Larsen RJ, Griffin S. The Satisfaction with Life Scale. Journal of Personality Assessment. 1985;49(1):71-5.
Lyubomirsky S, Lepper HS. A Measure of Subjective Happiness: Preliminary Reliability and Construct Validation. Social Indicators Research. 1999;46(2):137-55.
Diener E, Oishi S, Lucas RE. Subjective well-being: the science of happiness and life satisfaction. In: Lopez SJ, Snyder CR, editors. Oxford Handbook of Positive Psychology. Oxford Handbooks Online. Oxford University Press; 2012. P. 187-94.
Røysamb E, Nes RB, Czajkowski NO, Vassend O. Genetics, personality and wellbeing. A twin study of traits, facets and life satisfaction. Sci Rep. 2018;8(1):12298.
Ernst U, Baumgartner LP, Bauer UMM, Janssen GH. Improvement of quality of life in women using a low-dose desogestrel-containing contraceptive: results of an observational clinical evaluation. 2002;7(4):23843.
Helliwell JF, Layard R, Sachs J, De Neve JE, editors. World Happiness Report 2020. New York: Sustainable Development Solutions Network; 2020.
Smyth JM, Zawadzki MJ, Juth V, Sciamanna CN. Global life satisfaction predicts ambulatory affect, stress, and cortisol in daily life in working adults. J Behav Med. 2016;40(2):320-31.
Demeli M, Bayrak S, Pehlivanoğlu B. Effects of Adenosine on the Sleep-Wake Cycle. J Turk Sleep Med. 2022;9(3):190–8.
Walker MP, Stickgold R. Sleep-Dependent Learning and Memory Consolidation. Neuron. 2004 Sep;44(1):121-33.
Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci Med. 2010;71(5):1027-36.
Cirelli C, Tononi G. Is Sleep Essential? PloS Biology. 2008;6(8):e216.
McEwen BS. Physiology and Neurobiology of Stress and Adaptation: Central Role of the Brain. Physiol Rev. 2007;87(3):873-904
Akova İ, Duman EN, Sahar AE, Sümer EH. The Relationship Between Caffeine Consumption and Depression, Anxiety, Stress Level and Sleep Quality in Medical Students. J Turk Sleep Med. 2023;10(1):65-70.
Almojali AI, Almalki SA, Alothman AS, Masuadi EM, Alaqeel MK. The prevalence and association of stress with sleep quality among medical students. J Epidemiol Glob Health. 2017;7(3):169-74
Kjeldstadli K, Tyssen R, Finset A, Hem E, Gude T, Gronvold NT, et al. Life satisfaction and resilience in medical school – a six-year longitudinal, nationwide and comparative study. BMC Med Educ. 2006;6:48.
Shi M, Wang X, Bian Y, Wang L. The mediating role of resilience in the relationship between stress and life satisfaction among Chinese medical students: a cross-sectional study. BMC Med Educ. 2015;15:16.
Wang Q, Sun W, Wu H. Associations between academic burnout, resilience and life satisfaction among medical students: a three-wave longitudinal study. BMC Med Educ. 2022;22(1):248.
Ağargün MY, Kara H, Anlar O. [Validity and reliability of the Pittsburgh sleep quality index]. Turk Psikiyatri Dergisi. 1996;7(2):107-15.
Bekmezci̇M, Mert İS. [Turkish Validity and Reliability Study of the Life Satisfaction Scale]. Toros Üniversitesi İİSBF Sosyal Bilimler Dergisi. 2018;5(8):166-77.
Öner N, Le Compte A. [State-trait anxiety inventory manual]. Istanbul: Boğaziçi Üniversitesi Yayınılar; 1983.
Johnson KM, Simon N, Wicks M, Barr K, O’Connor K, Schaad D. Amount of Sleep, Daytime Sleepiness, Hazardous Driving, and Quality of Life of Second Year Medical Students. Acad Psychiatry. 2017;41(5):669-73.
Ball S, Bax A. Self-care in Medical Education. Acad Med. 2002;77(9):911-7.
Park BK. The Pittsburg Sleep Quality Index (PSQI) and Associated Factors in Middle-school Students: A Cross-sectional Study. Child Health Nurs Res. 2020;26(1):55-63.
Alotaibi AD, Alosaimi FM, Alajlan AA, Bin Abdulrahman KA. The relationship between sleep quality, stress, and academic performance among medical students. J Family Community Med. 2020;27(1):23–8.
Milovanska-Farrington S, Farrington S. Happiness, domains of life satisfaction, perceptions, and valuation differences across genders. Acta Psychol (Amst). 2022:230:103720.
Habibov N, Auchynnikava A, Luo R, Fan L. A healthy weight improves life satisfaction. Int J Health Plann Manage. 2018;34(1):396–413.
Baldursdottir K, McNamee P, Norton EC, Asgeirsdottir TL. Life satisfaction and body mass index: estimating the monetary value of achieving optimal body weight. Rev Econ Househ. 2023:1-32.
Machul M, Bieniak M, Chałdaś-Majdańska J, Bąk J, Chrzan-Rodak A, Mazurek P, et al. Lifestyle Practices, Satisfaction with Life and the Level of Perceived Stress of Polish and Foreign Medical Students Studying in Poland. Int J Environ Res. 2020;17(12):4445.
Guney S, Kalafat T, Boysan M. Dimensions of mental health: life satisfaction, anxiety and depression: a preventive mental health study in Ankara University students population. Procedia Soc Behav Sci. 2010;2(2):1210-3.
Odacı H, Çikrıkci Ö. Differences in Problematic Internet Use based on Depression, Anxiety, and Stress Levels. Addicta Turk J Addict. 2017;4:41-1.
Achar Fujii RN, Kobayasi R, Claassen Enns S, Zen Tempski P. Medical Students’ Participation in Extracurricular Activities: Motivations, Contributions, and Barriers. A Qualitative Study. Adv Med Educ Pract. 2022;13:1133-41.
Kötter T, Fuchs S, Heise M, Riemenschneider H, Sanftenberg L, Vajda C, et al. What keeps medical students healthy and well? A systematic review of observational studies on protective factors for health and well-being during medical education. BMC Med Educ. 2019;19(1):94.
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2024 Ervin Ozdemir, Yigit Yazarkan, Bilge Pehlivanoglu

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- The Author retains copyright in the Work, where the term “Work” shall include all digital objects that may result in subsequent electronic publication or distribution.
- Upon acceptance of the Work, the author shall grant to the Publisher the right of first publication of the Work.
- The Author shall grant to the Publisher and its agents the nonexclusive perpetual right and license to publish, archive, and make accessible the Work in whole or in part in all forms of media now or hereafter known under a Creative Commons Attribution 4.0 International License or its equivalent, which, for the avoidance of doubt, allows others to copy, distribute, and transmit the Work under the following conditions:
- Attribution—other users must attribute the Work in the manner specified by the author as indicated on the journal Web site; with the understanding that the above condition can be waived with permission from the Author and that where the Work or any of its elements is in the public domain under applicable law, that status is in no way affected by the license.
- The Author is able to enter into separate, additional contractual arrangements for the nonexclusive distribution of the journal's published version of the Work (e.g., post it to an institutional repository or publish it in a book), as long as there is provided in the document an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post online a prepublication manuscript (but not the Publisher’s final formatted PDF version of the Work) in institutional repositories or on their Websites prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. Any such posting made before acceptance and publication of the Work shall be updated upon publication to include a reference to the Publisher-assigned DOI (Digital Object Identifier) and a link to the online abstract for the final published Work in the Journal.
- Upon Publisher’s request, the Author agrees to furnish promptly to Publisher, at the Author’s own expense, written evidence of the permissions, licenses, and consents for use of third-party material included within the Work, except as determined by Publisher to be covered by the principles of Fair Use.
- The Author represents and warrants that:
- the Work is the Author’s original work;
- the Author has not transferred, and will not transfer, exclusive rights in the Work to any third party;
- the Work is not pending review or under consideration by another publisher;
- the Work has not previously been published;
- the Work contains no misrepresentation or infringement of the Work or property of other authors or third parties; and
- the Work contains no libel, invasion of privacy, or other unlawful matter.
- The Author agrees to indemnify and hold Publisher harmless from the Author’s breach of the representations and warranties contained in Paragraph 6 above, as well as any claim or proceeding relating to Publisher’s use and publication of any content contained in the Work, including third-party content.
Enforcement of copyright
The IJMS takes the protection of copyright very seriously.
If the IJMS discovers that you have used its copyright materials in contravention of the license above, the IJMS may bring legal proceedings against you seeking reparation and an injunction to stop you using those materials. You could also be ordered to pay legal costs.
If you become aware of any use of the IJMS' copyright materials that contravenes or may contravene the license above, please report this by email to contact@ijms.org
Infringing material
If you become aware of any material on the website that you believe infringes your or any other person's copyright, please report this by email to contact@ijms.org