Magnitude of Psychological Distress Among Medical and Non-Medical Students During the Late Phase of the COVID-19 Pandemic in West Bengal: A Cross-Sectional Study
DOI:
https://doi.org/10.5195/ijms.2024.2446Keywords:
Pandemics, Psychological Distress, Mental health services , Medical Students, Non-Medical Students, COVID-19 Pandemic, COVID-19, Depression, Anxiety, Knowledge-Attitude-Practice (KAP), Mental Health, Cross-Sectional Study, Student WellnessAbstract
Background: COVID-19 pandemic led to drastic changes worldwide affecting mental health of students. This study aimed to assess psychological distress due to COVID-19 in students during the late phase of pandemic and to establish correlation of academic course, socio-demographics, and knowledge-attitude-practices (KAP) with depression and anxiety.
Methods: A cross-sectional study was conducted in Kolkata, from March to April 2022 among undergraduate medical students and undergraduate students from engineering and general science colleges, via purposive and snowball sampling. Survey questionnaire was circulated via Google forms through social media. It included Patient Health Questionnaire-9, Generalized Anxiety Disorder-7, Fear of COVID-19 scale 2020, KAP regarding COVID-19 and socio-demographics. Data were analyzed using SPSS(Version 22.0) by estimating mean, standard deviation, median, interquartile range, and displayed by charts and tables. Mann-Whitney U test/non-parametric ANOVA and Chi-square tests were used for drawing statistical inferences. P-value of <0.05 was considered significant.
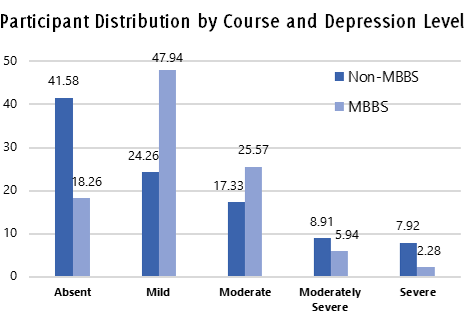
Results: A total of 421 responses were included: 219 medical and 202 non-medical students. Most participants were male (58.67%). Prevalence of depression was 58.42% among non-medical students and 81.73% among medical students. Prevalence of anxiety was 50.99% among non-medical students and 76.25% among medical students. Medical students had significantly better scores for knowledge and attitude (p=0.001 in both). Anxiety was influenced by residence (p=0.018), mode of travel (p=0.012), and having relatives or friends affected by COVID-19 (p=0.03).
Conclusion: High prevalence of depression and anxiety among college students, especially medical students, highlights the need for student wellness activities and better mental health services in colleges across India.
References
Cucinotta D, Vanelli M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020;91(1):157-60.
Gettleman J, Schultz K. Modi orders 3-week total lockdown for all 1.3 billion Indians. Available from:https://www.nytimes.com/2020/03/24/world/asia/india-coronavirus-lockdown.html ISSN 0362-4331. Last updated Mar 24, 2020; cited Nov 9, 2022.
Imran N, Haider II, Mustafa AB, Aamer I, Kamal Z, Rasool G, et al. The Hidden Crisis: COVID-19 and Impact on Mental Health of Medical Students in Pakistan. Middle East Curr Psychiatry. 2021;28(1):45.
Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of Depression Symptoms in US Adults Before and During the COVID-19 Pandemic. JAMA Netw Open. 2020;3(9):e2019686.
Mohammed S, Tharayil H, Gopakumar S, George C. Pattern and Correlates of Depression among Medical Students: An 18 Month Follow-Up Study. Indian J Psychol Med. 2020;42(2):116-21.
India Briefing. How India is Managing COVID-19 in 2022: Transition to the Workplace, Vaccine Program Expanded. Available from: https://www.india-briefing.com/news/india-COVID-19-vaccine-program-best-practice-employers-2022-23998.html/. Last updated Mar 24, 2022 ; cited Nov 9, 2022.
Shailaja B, Singh H, Chaudhury S, Thyloth M. COVID-19 pandemic and its aftermath: Knowledge, attitude, behavior, and mental health-care needs of medical undergraduates. Ind Psychiatry J. 2020;29(1):51-60.
Saraswathi I, Saikarthik J, Senthil Kumar K, Madhan Srinivasan K, Ardhanaari M, Gunapriya R. Impact of COVID-19 outbreak on the mental health status of undergraduate medical students in a COVID-19 treating medical college: a prospective longitudinal study. PeerJ. 2020;8:e10164.
Bhowmick S, Parolia S, Jana S, Kundu D, Choudhury D, Das N, et al. A Study on the Anxiety Level and Stress during Covid19 Lockdown among the General Population of West Bengal, India- A Must Know for Primary Care Physicians. J Family Med Prim Care. 2021;10(2):978-84.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a Brief Depression Severity Measure. J Gen Intern Med. 2001;16(9):606-13.
Spitzer RL, Kroenke K, Williams JB, Lowe B. A Brief Measure for Assessing Generalized Anxiety Disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092-7.
De Man J, Absetz P, Sathish T, Desloge A, Haregu T, Oldenburg B, et al. Are the PHQ-9 and GAD-7 Suitable for Use in India? A Psychometric Analysis. Front Psychol. 2021;12:676398.
Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The Fear of COVID-19 Scale: Development and Initial Validation. Int J Ment Health Addict. 2022;20(3):1537-45.
Chaudhary AP, Sonar NS, TR J, Banerjee M, Yadav S. Impact of the COVID-19 Pandemic on the Mental Health of College Students in India: Cross-sectional Web-Based Study. JMIRx Med. 2021;2(3):e28158.
Lee M, Kang BA, You M. Knowledge, Attitudes, and Practices (KAP) toward COVID-19: A Cross-sectional Study in South Korea. BMC Public Health. 2021;21(1):295.
Shreevastava AK, Mavai M, Mittal PS, Verma R, Kaur D, Bhandari B. Assessment of the psychological impact of COVID-19 pandemic on undergraduate medical students in India. J Edu Health Promot2022;11:214.
Mishra J, Samanta P, Panigrahi A, Dash K, Behera MR, Das R. Mental Health Status, Coping Strategies during COVID-19 Pandemic among Undergraduate Students of Healthcare Profession. Int J Ment Health Addict. 2023;21(1):562-74.
Zheng X, Guo Y, Yang H, Luo L, Ya B, Xu H, et al. A Cross-Sectional Study on Mental Health Problems of Medical and Nonmedical Students in Shandong During the COVID-19 Epidemic Recovery Period. Front. Psychiatry 2021;12:1-9.
Pradeep BS, Gururaj G, Varghese M, Benegal V, Rao GN, Sukumar GM. National Mental Health Survey of India, 2016 - Rationale, Design and Methods. PLoS ONE. 2018;13(10):e0205096.
Rotenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, et al. Prevalence of Depression, Depressive Symptoms, and Suicidal Ideation Among Medical Students: A Systematic Review and Meta-Analysis. JAMA. 2016;316(21):2214–36.
Quek TT, Tam WW, Tran BX, Zhang M, Zhang Z, Ho CS, et al. The Global Prevalence of Anxiety Among Medical Students: A Meta-Analysis. Int J Environ Res Public Health. 2019;16(15):2735.
Verma H, Verma G, Kumar P. Depression, Anxiety, and Stress during Times of COVID-19: An Analysis of Youngsters Studying in Higher Education in India. Rev SocionetworkStrateg. 2021;15(2):471-88.
Islam MA, Barna SD, Raihan H, Khan MNA, Hossain MT. Depression and Anxiety among University Students during the COVID-19 Pandemic in Bangladesh: A Web-based Cross-sectional Survey. PLoS ONE. 2020;15(8) :e0238162.
Son C, Hegde S, Smith A, Wang X, Sasangohar F, et al. Effects of COVID-19 on College Students’ Mental Health in the United States: Interview Survey Study. J Med Internet Res. 2020;22(9):e21279.
Awadalla NJ, Alsabaani AA, Alsaleem MA, Alsaleem SA, Alshaikh AA, Al-Fifi SH, et al. Increased Mental Stress among Undergraduate Medical Students in South-Western Saudi Arabia during the COVID-19 Pandemic. PeerJ 2022;10:e13900.
Gallagher MW, Zvolensky MJ, Long LJ, Rogers AH, Garey L. The Impact of COVID-19 Experiences and Associated Stress on Anxiety, Depression, and Functional Impairment in American Adults. Cognit Ther Res. 2020;44(6):1043-51.
Adli I, Widyahening IS, Lazarus G, Phowira J, Baihaqi LA, Ariffandi B, et al. Knowledge, Attitude, and Practice related to the COVID-19 Pandemic among Undergraduate Medical Students in Indonesia: A Nationwide Cross Sectional Study. PLoS ONE. 2022;17(1):e0262827.
Chan SS, So WK, Wong DC, Lee AC, Tiwari A. Improving Older Adults’ Knowledge and Practice of Preventive Measures through a Telephone Health Education during the SARS Epidemic in Hong Kong: A Pilot Study. Int J Nurs Stud. 2007;44:1120–7.
Moore KA, Lucas JJ. COVID-19 Distress and Worries: The Role of Attitudes, Social Support, and Positive Coping during Social Isolation. Psychol Psychother. 2021; 94(2):365-70.
Khan K, Li Y, Liu S, Li C. Psychological Distress and Trust in University Management Among International Students During the COVID-19 Pandemic. Front. Psychol. 2021;12:679661.
Saali A, Stanislawski ER, Kumar V, Chan C, Hurtado A, Pietrzak RH, et al. The Psychiatric Burden on Medical Students in New York City Entering Clinical Clerkships during the COVID-19 Pandemic. Psychiatr Q. 2022;93(2):419-34.
Horwitz AG, Hill RM, King CA. Specific Coping Behaviors in Relation to Adolescent Depression and Suicidal Ideation. J Adolesc. 2011;34(5):1077-85.
Arjun MC, Singh AK, Roy P, Ravichandran M, Mandal S, Pal D, et al. Long COVID Following Omicron Wave in Eastern India—A Retrospective Cohort Study. J Med Virol. 2022;95:e28214.
Steimle LN, Sun Y, Johnson L, Besedes T, Mokhtarian P, Nazzal D. Students' Preferences for Returning to Colleges and Universities during the COVID-19 Pandemic: A Discrete Choice Experiment. SocioeconPlann Sci. 2022;82:101266.
Mandal A, Ghosh A, Sengupta G, Bera T, Das N, Mukherjee S. Factors Affecting The Performance Of Undergraduate Medical Students: A Perspective. Indian J Community Med. 2012;37(2):126-9.
Woolery A, Myers H, Sternlieb B, Zeltzer L. A Yoga Intervention for Young Adults with Elevated Symptoms of Depression. Altern Ther Health Med. 2004;10(2):60-3.
Haglund ME, aan het Rot M, Cooper NS, Nestadt PS, Muller D, Southwick SM, et al. Resilience in the Third Year of Medical School: A Prospective Study of the Associations between Stressful Events Occurring during Clinical Rotations and Student Well-being. Acad Med. 2009;84(2):258–68.
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Udisa Das, Arunima Ganguly , Dibakar Haldar, Asish Mukhopadhyay

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- The Author retains copyright in the Work, where the term “Work” shall include all digital objects that may result in subsequent electronic publication or distribution.
- Upon acceptance of the Work, the author shall grant to the Publisher the right of first publication of the Work.
- The Author shall grant to the Publisher and its agents the nonexclusive perpetual right and license to publish, archive, and make accessible the Work in whole or in part in all forms of media now or hereafter known under a Creative Commons Attribution 4.0 International License or its equivalent, which, for the avoidance of doubt, allows others to copy, distribute, and transmit the Work under the following conditions:
- Attribution—other users must attribute the Work in the manner specified by the author as indicated on the journal Web site; with the understanding that the above condition can be waived with permission from the Author and that where the Work or any of its elements is in the public domain under applicable law, that status is in no way affected by the license.
- The Author is able to enter into separate, additional contractual arrangements for the nonexclusive distribution of the journal's published version of the Work (e.g., post it to an institutional repository or publish it in a book), as long as there is provided in the document an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post online a prepublication manuscript (but not the Publisher’s final formatted PDF version of the Work) in institutional repositories or on their Websites prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. Any such posting made before acceptance and publication of the Work shall be updated upon publication to include a reference to the Publisher-assigned DOI (Digital Object Identifier) and a link to the online abstract for the final published Work in the Journal.
- Upon Publisher’s request, the Author agrees to furnish promptly to Publisher, at the Author’s own expense, written evidence of the permissions, licenses, and consents for use of third-party material included within the Work, except as determined by Publisher to be covered by the principles of Fair Use.
- The Author represents and warrants that:
- the Work is the Author’s original work;
- the Author has not transferred, and will not transfer, exclusive rights in the Work to any third party;
- the Work is not pending review or under consideration by another publisher;
- the Work has not previously been published;
- the Work contains no misrepresentation or infringement of the Work or property of other authors or third parties; and
- the Work contains no libel, invasion of privacy, or other unlawful matter.
- The Author agrees to indemnify and hold Publisher harmless from the Author’s breach of the representations and warranties contained in Paragraph 6 above, as well as any claim or proceeding relating to Publisher’s use and publication of any content contained in the Work, including third-party content.
Enforcement of copyright
The IJMS takes the protection of copyright very seriously.
If the IJMS discovers that you have used its copyright materials in contravention of the license above, the IJMS may bring legal proceedings against you seeking reparation and an injunction to stop you using those materials. You could also be ordered to pay legal costs.
If you become aware of any use of the IJMS' copyright materials that contravenes or may contravene the license above, please report this by email to contact@ijms.org
Infringing material
If you become aware of any material on the website that you believe infringes your or any other person's copyright, please report this by email to contact@ijms.org







