Prevalence and Burden of Disorders of Gut-Brain Interaction Among UK Medical Students
DOI:
https://doi.org/10.5195/ijms.2024.2449Keywords:
Disorders of Gut‐Brain Interaction, Functional Gastrointestinal Disorders, Psychological Distress, Burnout , Gut-Brain Interaction, Medical Students, Prevalence, Health Surveys, Questionnaires, Anxiety, Depression, Eating Disorders, Quality of Life, Burnout, Professional, Somatic Symptom Disorders, Rome IV Criteria, Irritable Bowel Syndrome, Functional Dyspepsia, Healthcare Utilization, United Kingdom, Cross-Sectional Studies, Mental HealthAbstract
Background: Disorders of Gut-Brain Interaction (DGBI) affect 40% of the general population and are associated with substantial health impairment. Medical students reportedly have among the highest rates of DGBI, although data is mainly from Asia and Africa. We addressed this issue within a UK-based university.
Methods: An online survey was completed by 378 of 1621 medical students. Demographics, medical history, and gastrointestinal symptoms were collected, the latter using a modified Rome IV questionnaire to determine the presence of DGBI symptoms over the last 3 months. Additional validated questionnaires screened for somatization, psychological distress, eating disorders, quality of life, and burnout.
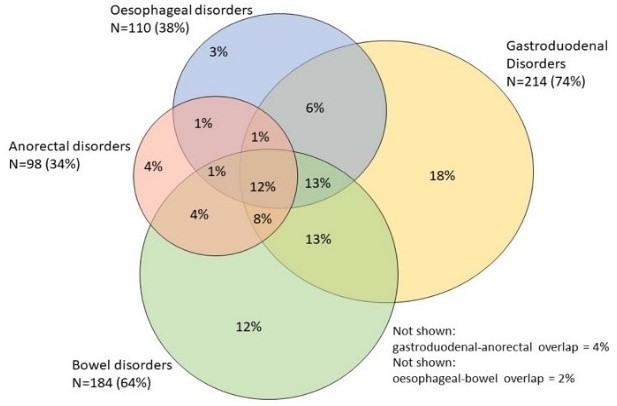
Results: DGBI were present in 76% (n=289/378), of which two-of-three had multiple affected sites. The most frequent DGBI were gastroduodenal (57%), followed by bowel (49%), esophageal (29%), and anorectal (26%) disorders. Approximately 50% of students with DGBI experienced painful gastrointestinal symptoms at least one day/week. Students with DGBI, compared to those without, had significantly higher anxiety and depression scores, increased somatic symptom reporting, reduced mental and physical quality of life, poorer eating habits, and more frequent medication use (p-values, all<0.05). They were also at significantly higher risk of burnout, through study exhaustion and disengagement. The greatest health impairment was seen in those with multiple, painful, DGBI. Only 23% and 5% of students with DGBI had consulted a primary care provider and gastroenterologist, respectively.
Conclusion: Medical students commonly experience DGBI and associated health burden, yet infrequently seek help. Greater awareness may lead to increased support, improved health, and better study engagement.
References
Drossman DA, Hasler WL. Rome IV—Functional GI Disorders: Disorders of Gut-Brain Interaction. Gastroenterology. 2016;150(6):1257-61.
Sperber AD, Bangdiwala SI, Drossman DA, Ghoshal UC, Simren M, Tack J, et al. Worldwide Prevalence and Burden of Functional Gastrointestinal Disorders, Resultsof Rome Foundation Global Study. Gastroenterology. 2021;160(1):99-114.e3.
Aziz I, Palsson OS, Törnblom H, Sperber AD, Whitehead WE, Simrén M. The prevalence and impact of overlapping Rome IV-diagnosed functional gastrointestinal disorders on somatization, quality of life, and healthcare utilization: A cross-sectional general populationstudy in threecountries. Am J Gastroenterol. 2018;113(1):86-96.
Staller K, Abber SR, Burton Murray H. The intersection between eating disorders and gastrointestinal disorders: a narrative review and practical guide. Lancet Gastroentero lHepatol. 2023;8(6):565-78.
Molodynski A, Lewis T, Kadhum M, Farrell SM, LemtiriChelieh M, Falcão De Almeida T, et al. Cultural variations in wellbeing, burnout and substance use amongst medical students in twelve countries. Int Rev Psychiatry. 2021;33(1-2):37-42.
Kadhum M, Ayinde OO, Wilkes C, Chumakov E, Dahanayake D, Ashrafi A, et al. Wellbeing, burnout and substance use amongst medical students: A summary of results from nine countries. Int J Soc Psychiatry. 2022;68(6):1218-22.
Palsson OS, Whitehead WE, Van Tilburg MAL, Chang L, Chey W, Crowell MD, et al. Development and Validation of the Rome IV Diagnostic Questionnaire for Adults. Gastroenterology. 2016;150(6):1481-91.
Morgan JF, Reid F, Lacey JH. The SCOFF Questionnaire: Assessmentof a New Screening Tool for Eating Disorders. BMJ. 1999;319(7223):1467-8.
Hill LS, Reid F, Morgan JF, Lacey JH. SCOFF, the development of an eating disorder screening questionnaire. Int J Eat Disord. 2010;43(4):344-51.
Spiller RC, Humes DJ, Campbell E, Hastings M, Neal KR, Dukes GE, et al. The Patient Health Questionnaire 12 Somatic Symptom scale as a predictor ofsymptomseverity and consultingbehaviour in patientswith irritable bowelsyndrome and symptomatic diverticular disease. Aliment Pharmacol Ther. 2010;32(6):811-20.
Zigmond AS, Snaith RP. The Hospital Anxiety and DepressionScale. Acta Psychiatr Scand. 1983;67(6):361-70.
Ware JE, Kosinski M, Dewey JE, Gandek B. How to score and interpret single-item health status measures: a manual for users of the SF-8 health survey. Lincoln, RI: Quality Metric Incorporated. 2001;15(10):5.
Demerouti E, Bakker AB. The Oldenburg Burnout Inventory: A good alternative to measure burnout and engagement. Handbook of stress and burnout in health care. 2008;65(7):1-25.
Luo Y, Camey SA, Bangdiwala SI, Palsson OS, Sperber AD, Keefer LA. Global patterns of prescription pain medication usage in disorders of gut–braininteractions. Neurogastroenterol Motil. 2023;35(1):e14457.
Zia JK, Lenhart A, Yang PL, Heitkemper MM, Baker J, Keefer L, et al. Risk Factors for Abdominal Pain-Related Disorders of Gut-Brain Interaction in Adults and Children: A Systematic Review. Gastroenterology. 2022;163(4):995-1023.e3.
Tan Y-M, Goh KL, Muhidayah R, Ooi CL, Salem O. Prevalence of irritable bowel syndrome in young adult Malaysians: A survey among medical students. J Gastroenterol Hepatol. 2003;18(12):1412-6.
Gallas S, Knaz H, Methnani J, Maatallah Kanzali M, Koukane A, Bedoui MH, et al. Prevalence and risk factors of functional gastrointestinal disorders in early period medical students: a pilot study in Tunisia. Libyan J Med. 2022;17(1).
Jafri W, Yakoob J, Jafri N, Islam M, Ali QM. Frequency of irritable bowel syndrome in college students. J Ayub Med Coll Abbottabad. 2005;17(4):9.
Shahaf-Oren B, Madan I, Henderson C. “A lot of medical students, their biggest fear is failing at being seen to be a functional human”: disclosure and help-seeking decisions by medical students with health problems. BMC Med Educ. 2021;21(1):1-599.
Menon V, Sarkar S, Kumar S. A cross-sectional analysis of barriers to health-care seeking among medical students across training period. J Ment Health Hum Be. 2017;22(2):97-103.
Simons J, Shajee U, Palsson O, Simren M, Sperber AD, Törnblom H, et al. Disorders of gut-brain interaction: Highly prevalent and burdensome yet under-taught within medical education. United European Gastroenterol J. 2022;10(7):736-44.
Farrell SM, Kadhum M, Lewis T, Singh G, Penzenstadler L, Molodynski A. Wellbeing and burnout amongst medical students in England. Int Rev Psychiatry. 2019;31(7-8):579-83.
Farrell SM, Molodynski A, Cohen D, Grant AJ, Rees S, Wullshleger A, et al. Wellbeing and burnout among medical students in Wales. Int Rev Psychiatry. 2019;31(7-8):613-8.
Erschens R, Keifenheim KE, Herrmann-Werner A, Loda T, Schwille-Kiuntke J, Bugaj TJ, et al. Professional burnout among medical students: Systematic literature review and meta-analysis. Med Teach. 2019;41(2):172-83.
Hod K, Melamed S, Dekel R, Maharshak N, Sperber AD. Burnout, butnotjobstrain, isassociatedwith irritable bowelsyndrome in workingadults. J Psychosom Res. 2020;134:110121-.
Patacchioli FR, Angelucci L, Dell’Erba G, Monnazzi P, Leri O. Actual stress, psychopathology and salivary cortisol levels in the irritable bowelsyndrome (IBS). J Endocrinol Invest. 2001;24(3):173-7.
Jahrami H, Sater M, Abdulla A, FarisMeA-I, AlAnsari A. Eatingdisordersriskamong medical students: a global systematicreview and meta-analysis. Eat Weight Disord. 2019;24(3):397-410.
Hodkinson A, Zhou A, Johnson J, Geraghty K, Riley R, Zhou A, et al. Associations of physician burnout with career engagement and quality of patient care: systematic review and meta-analysis. BMJ. 2022;378:e070442.
Goyal O, Nohria S, Dhaliwal AS, Goyal P, Soni RK, Chhina RS, et al. Prevalence, overlap, and risk factors for Rome IV functional gastrointestinal disorders among college students in northern India. Indian J Gastroenterol. 2021;40(2):144-53.
Bogowicz P, Ferguson J, Gilvarry E, Kamali F, Kaner E, Newbury-Birch D. Alcohol and other substance use among medical and law students at a UK university: a cross-sectional questionnaire survey. Postgrad Med J. 2018;94(1109):131-6.
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2024 Lydia C Brown, Imran Aziz

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- The Author retains copyright in the Work, where the term “Work” shall include all digital objects that may result in subsequent electronic publication or distribution.
- Upon acceptance of the Work, the author shall grant to the Publisher the right of first publication of the Work.
- The Author shall grant to the Publisher and its agents the nonexclusive perpetual right and license to publish, archive, and make accessible the Work in whole or in part in all forms of media now or hereafter known under a Creative Commons Attribution 4.0 International License or its equivalent, which, for the avoidance of doubt, allows others to copy, distribute, and transmit the Work under the following conditions:
- Attribution—other users must attribute the Work in the manner specified by the author as indicated on the journal Web site; with the understanding that the above condition can be waived with permission from the Author and that where the Work or any of its elements is in the public domain under applicable law, that status is in no way affected by the license.
- The Author is able to enter into separate, additional contractual arrangements for the nonexclusive distribution of the journal's published version of the Work (e.g., post it to an institutional repository or publish it in a book), as long as there is provided in the document an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post online a prepublication manuscript (but not the Publisher’s final formatted PDF version of the Work) in institutional repositories or on their Websites prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. Any such posting made before acceptance and publication of the Work shall be updated upon publication to include a reference to the Publisher-assigned DOI (Digital Object Identifier) and a link to the online abstract for the final published Work in the Journal.
- Upon Publisher’s request, the Author agrees to furnish promptly to Publisher, at the Author’s own expense, written evidence of the permissions, licenses, and consents for use of third-party material included within the Work, except as determined by Publisher to be covered by the principles of Fair Use.
- The Author represents and warrants that:
- the Work is the Author’s original work;
- the Author has not transferred, and will not transfer, exclusive rights in the Work to any third party;
- the Work is not pending review or under consideration by another publisher;
- the Work has not previously been published;
- the Work contains no misrepresentation or infringement of the Work or property of other authors or third parties; and
- the Work contains no libel, invasion of privacy, or other unlawful matter.
- The Author agrees to indemnify and hold Publisher harmless from the Author’s breach of the representations and warranties contained in Paragraph 6 above, as well as any claim or proceeding relating to Publisher’s use and publication of any content contained in the Work, including third-party content.
Enforcement of copyright
The IJMS takes the protection of copyright very seriously.
If the IJMS discovers that you have used its copyright materials in contravention of the license above, the IJMS may bring legal proceedings against you seeking reparation and an injunction to stop you using those materials. You could also be ordered to pay legal costs.
If you become aware of any use of the IJMS' copyright materials that contravenes or may contravene the license above, please report this by email to contact@ijms.org
Infringing material
If you become aware of any material on the website that you believe infringes your or any other person's copyright, please report this by email to contact@ijms.org







