Healthcare Workers’ Perceptions of Patient Safety Culture in United States Hospitals: A Systematic Review and Meta-Analysis
DOI:
https://doi.org/10.5195/ijms.2024.2560Keywords:
Patient safety, Patient safety culture, Hospital survey on patient safety culture, Systematic Review, Meta-Analysis, Healthcare Professionals, Medical Errors, Teamwork, Nonpunitive Response to Error, Handoffs and Transitions, Safety Improvement InterventionsAbstract
Background: Despite leading in healthcare spending, the United States sees only marginal improvements in patient outcomes among developed nations. Assessing patient safety culture (PSC) through the Hospital Survey on Patient Safety Culture (HSOPSC) provides insights into overall patient safety and attitudes toward medical errors. This study aims to examine PSC in U.S. hospitals across professional categories via a systematic review and meta-analysis of published literature.
Methods: Embase, PubMed (Medline), Web of Science, Scopus, and AHRQ’s Bibliography were consulted for identifying studies. A total of 31 articles met the eligibility criteria for inclusion, which garnered 608,443 survey participants in a national population of hospital healthcare professionals. For each professional category of PSC, a fixed and random-effects meta-analysis was performed, and a subgroup analysis was also conducted to measure differences in perceptions of PSC based on type of healthcare professional.
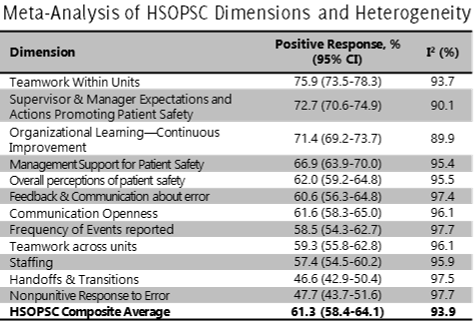
Results: The HSOPSC composite average across all the studies was 61.3% positive responsiveness, indicating a need for improvement in patient safety. “Teamwork within units” had the highest positive PSC perception while “nonpunitive response to error” and “handoffs and transitions” scored the lowest. Furthermore, healthcare trainees and physicians seemed to have overall worse perceptions of patient safety culture compared to other professional subgroups, indicating the potential impacts of inexperience and a culpability culture on patient safety and medical error in hospitals.
Discussion: To strengthen weak aspects of patient safety culture, hospitals should implement interventions such as teamwork training and error-reporting systems, thereby enhancing patient safety measures and reducing medical errors.
References
McElroy LM, Woods DM, Yanes AF, Skaro AI, Daud A, Curtis T, et al. Applying the WHO conceptual framework for the International Classification for Patient Safety to a surgical population. Int J Qual Health Care. 2016;28(2):166-74.
Green B, Tsiroyannis C, Brennan P. Human factors - recognising and minimising errors in our day to day practice. Oral Dis. 2015;22(1):19-22.
Kohn LT, Corrigan J, Donaldson MS. To err is human: building a safer health system. Washington: National Academy Press; 2000.
Lark ME, Kirkpatrick K, Chung KC. Patient safety movement: history and future directions. J Hand Surg. 2018;43(2):174-8.
Clancy CM. Ten years after To Err Is Human. Am J Med Qual. 2009;24(6):525-8.
Auraaen A, Slawomirski L, Klazinga N. The economics of patient safety in primary and ambulatory care. OECD Health Working Papers. 2018.
Organisation for Economic Co-operation and Development, OECD. The economics of patient safety. OECD Health Working Papers. 2022.
Kruk ME, Gage AD, Joseph NT, Danaei G, García-Saisó S, Salomon JA. Mortality due to low-quality health systems in the universal health coverage era: a systematic analysis of amenable deaths in 137 countries. Lancet. 2018;392(10160):2203-12.
DiCuccio MH. The relationship between patient safety culture and patient outcomes. J Patient Saf. 2015;11(3):135-42.
Birkmeyer NJO, Finks JF, Greenberg CK, McVeigh A, English WJ, Carlin A, et al. Safety culture and complications after bariatric surgery. Ann Surg. 2013;257(2):260-5.
Fan CJ, Pawlik TM, Daniels T, Vernon N, Banks K, Westby P, et al. Association of safety culture with surgical site infection outcomes. J Am Coll Surg. 2016;222(2):122-8.
Sorra JS, Dyer N. Multilevel psychometric properties of the AHRQ hospital survey on patient safety culture. BMC Health Serv Res. 2010;10(1).
Reis CT, Paiva SG, Sousa P. The patient safety culture: a systematic review by characteristics of Hospital Survey on Patient Safety Culture dimensions. Int J Qual Health Care. 2018;30(9):660-77.
Okuyama JHH, Galvao TF, Silva MT. Healthcare professional’s perception of patient safety measured by the Hospital Survey on Patient Safety Culture: a systematic review and meta-analysis. Sci World J. 2018;2018:1-11.
Lawati MHAL, Dennis S, Short SD, Abdulhadi NN. Patient safety and safety culture in primary health care: a systematic review. BMC Fam Pract. 2018;19(1):1-12.
Nieva VF, Sorra J. Safety culture assessment: a tool for improving patient safety in healthcare organizations. Qual Saf Health Care. 2003;12 Suppl 2:ii17-23.
Waterson P, Carman EM, Manser T, Hammer A. Hospital Survey on Patient Safety Culture (HSPSC): a systematic review of the psychometric properties of 62 international studies. BMJ Open. 2019;9(9):e026896.
Agency for Healthcare Research & Quality. Hospital survey on patient safety culture. Available from: https://www.ahrq.gov/sops/surveys/hospital/index.html.
Martin AB, Hartman M, Benson J, Catlin A, The National Health Expenditure Accounts Team. National health care spending in 2021: decline in federal spending outweighs greater use of health care. Health Aff (Millwood). 2022;42(1).
Shrank WH, Rogstad TL, Parekh N. Waste in the US health care system. JAMA. 2019;322(15).
Papanicolas I, Woskie LR, Jha AK. Health care spending in the United States and other high-income countries. JAMA. 2018;319(10):1024-39.
Radley DC, Williams RD II, Gunja MZ, Baumgartner JC, Gumas ED. Americans, no matter the state they live in, die younger than people in many other countries. Available from: https://www.commonwealthfund.org/blog/2022/americans-no-matter-state-they-live-die-younger-people-many-other-countries. Last updated: Aug 11, 2022.
Elliott JH, Synnot A, Turner T, Simmonds M, Akl EA, McDonald S, et al. Living systematic review: 1. introduction—the why, what, when, and how. J Clin Epidemiol. 2017;91:23-30.
Kelly SE, Curran JA, Tricco AC. Managing unmanageable loads of evidence: are living reviews the answer? JBI Evid Synth. 2022;20(1):1-2.
Tetzlaff J, Page M, Moher D. The PRISMA 2020 statement: development of and key changes in an updated guideline for reporting systematic reviews and meta-analyses. Value Health. 2020;23(10):S312-3.
Halligan M, Zecevic A. Safety culture in healthcare: a review of concepts, dimensions, measures and progress. BMJ Qual Saf. 2011;20(4):338-43.
Mohammed F, Taddele M, Gualu T. Patient safety culture and associated factors among health care professionals at public hospitals in Dessie town, north east Ethiopia, 2019. PLoS One. 2021;16(2):e0245966.
Agency for Healthcare Research and Quality. Hospital survey on patient safety culture: user’s guide. Available from: https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/quality-patient-safety/patientsafetyculture/hospital/userguide/hospitalusersguide.pdf.
Tufanaru C, Munn Z, Aromataris E, Campbell J, Hopp L, editors. JBI manual for evidence synthesis. Adelaide: Joanna Briggs Institute; 2020. Available from: https://synthesismanual.jbi.global.
Munn Z, Moola S, Riitano D, Lisy K. The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence. Int J Health Policy Manag. 2014;3(3):123-8.
Barker TH, Migliavaca CB, Stein C, Colpani V, Falavigna M, Aromataris E, et al. Conducting proportional meta-analysis in different types of systematic reviews: a guide for synthesisers of evidence. BMC Med Res Methodol. 2021;21(1).
Tawfik GM, Dila KAS, Mohamed MYF, Tam DNH, Kien ND, Ahmed AM, et al. A step by step guide for conducting a systematic review and meta-analysis with simulation data. Trop Med Health. 2019;47(1):1-9.
Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1(2):97-111.
Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539-58.
Agency for Healthcare Research and Quality. SOPS bibliography. Available from: https://www.ahrq.gov/sops/bibliography/index.html.
Singer SJ, Baker LC. Relationship of safety climate and safety performance in hospitals. Acad Manag Proc. 2007;2007(1):1-6.
Jasti H, Sheth H, Verrico M, Perera S, Bump G, Simak D, et al. Assessing patient safety culture of internal medicine house staff in an academic teaching hospital. J Grad Med Educ. 2009;1(1):139-45.
Profit J, Lee HC, Sharek PJ, Kan P, Nisbet CC, Thomas EJ, et al. Comparing NICU teamwork and safety climate across two commonly used survey instruments. BMJ Qual Saf. 2015;25(12):954-61.
Bump GM, Calabria J, Gosman G, Eckart C, Metro DG, Jasti H, et al. Evaluating the clinical learning environment: resident and fellow perceptions of patient safety culture. J Grad Med Educ. 2015;7(1):109-12.
Blegen MA, Sehgal NL, Alldredge BK, Gearhart S, Auerbach AA, Wachter RM. Republished paper: improving safety culture on adult medical units through multidisciplinary teamwork and communication interventions: the TOPS project. Postgrad Med J. 2010;86(1022):729-33.
Campbell EG, Singer S, Kitch BT, Iezzoni LI, Meyer GS. Patient safety climate in hospitals: act locally on variation across units. Jt Comm J Qual Patient Saf. 2010;36(7):319-26.
DuPree E, Anderson R, McEvoy MD, Brodman M. Professionalism: a necessary ingredient in a culture of safety. Jt Comm J Qual Patient Saf. 2011;37(10):447-55.
Jones KJ, Skinner AM, High R, Reiter-Palmon R. A theory-driven, longitudinal evaluation of the impact of team training on safety culture in 24 hospitals. BMJ Qual Saf. 2013;22(5):394-404.
Mardon RE, Khanna K, Sorra J, Dyer N, Famolaro T. Exploring relationships between hospital patient safety culture and adverse events. J Patient Saf. 2010;6(4):226-32.
Ulrich B, Kear T. Patient safety culture in nephrology nurse practice settings: initial findings. Nephrol Nurs J. 2015;41(5):459-75.
Wagner C, Smits M, Sorra J, Huang CC. Assessing patient safety culture in hospitals across countries. Int J Qual Health Care. 2013;25(3):213-21.
Wu Y, Fujita S, Seto K, Ito S, Matsumoto K, Huang CC, et al. The impact of nurse working hours on patient safety culture: a cross-national survey including Japan, the United States and Chinese Taiwan using the Hospital Survey on Patient Safety Culture. BMC Health Serv Res. 2013;13(1).
Gampetro PJ, Segvich JP, Jordan N, Velsor-Friedrich B, Burkhart L. Perceptions of pediatric hospital safety culture in the United States. J Patient Saf. 2019.
Noureldin M, Noureldin MA. Reporting frequency of three near-miss error types among hospital pharmacists and associations with hospital pharmacists’ perceptions of their work environment. Res Social Adm Pharm. 2021;17(2):381-7.
Lozito M, Whiteman K, Swanson-Biearman B, Barkhymer M, Stephens K. Good catch campaign: improving the perioperative culture of safety. AORN J. 2018;107(6):705-14.
Smith SA, Yount N, Sorra J. Exploring relationships between hospital patient safety culture and Consumer Reports safety scores. BMC Health Serv Res. 2017;17(1).
Sorra J, Khanna K, Dyer N, Mardon R, Famolaro T. Exploring relationships between patient safety culture and patients’ assessments of hospital care. J Patient Saf. 2012;8(3):131-9.
MacKay MM, Jordan KS, Powers K, Munn LTM. Improving reporting culture through daily safety huddle. Qual Manag Health Care. 2023.
Campione J, Famolaro T. Promising practices for improving hospital patient safety culture. Jt Comm J Qual Patient Saf. 2018;44(1):23-32.
Lee SE, Dahinten VS. The enabling, enacting, and elaborating factors of safety culture associated with patient safety: a multilevel analysis. J Nurs Scholarsh. 2020;52(5):544-52.
Jones KJ, Skinner A, Xu L, Sun J, Mueller K. The AHRQ Hospital Survey on Patient Safety Culture: a tool to plan and evaluate patient safety programs. Adv Patient Saf. 2008.
Hefner JL, Hilligoss B, Knupp A, Bournique J, Sullivan J, Adkins E, et al. Cultural transformation after implementation of crew resource management: is it really possible? Am J Med Qual. 2016;32(4):384-90.
Klingner J, Moscovice I, Tupper J, Coburn A, Wakefield M. Implementing patient safety initiatives in rural hospitals. J Rural Health. 2009;25(4):352-7.
Lin DM, Carson KA, Lubomski LH, Wick EC, Pham JC. Statewide collaborative to reduce surgical site infections: results of the Hawaii surgical unit-based safety program. J Am Coll Surg. 2018;227(2):189-197.e1.
Hook JN, Boan D, Davis DE, Aten JD, Ruiz JM, Maryon T. Cultural humility and hospital safety culture. J Clin Psychol Med Settings. 2016;23(4):402-9.
Pimentel MPT, Choi S, Fiumara K, Kachalia A, Urman RD. Safety culture in the operating room. J Patient Saf. 2017.
Bump GM, Coots N, Liberi CA, Minnier TE, Phrampus PE, Gosman G, et al. Comparing trainee and staff perceptions of patient safety culture. Acad Med. 2017;92(1):116-22.
Jones F, Podila P, Powers C. Creating a culture of safety in the emergency department. J Nurs Adm. 2013;43(4):194-200.
Armellino D, Quinn Griffin MT, Fitzpatrick JJ. Structural empowerment and patient safety culture among registered nurses working in adult critical care units. J Nurs Manag. 2010;18(7):796-803.
Legg JS, Aaron L, Dempsey MC. Patient safety perceptions among vascular interventional technologists. Radiol Technol. 2013;84(2):106-11.
Hannah KL, Schade CP, Lomely DR, Ruddick P, Bellamy GR. Hospital administrative staff vs. nursing staff responses to the AHRQ Hospital Survey on Patient Safety Culture. Adv Patient Saf. 2008.
Marsteller JA, Wen M, Hsu YJ, Bauer L, Schwann NM, Young CJ, et al. Safety culture in cardiac surgical teams: data from five programs and national surgical comparison. Ann Thorac Surg. 2015;100(6):2182-9.
Sehgal NL, Fox M, Vidyarthi AR, Sharpe BA, Gearhart S, Bookwalter T, et al. A multidisciplinary teamwork training program: the triad for optimal patient safety (TOPS) experience. J Gen Intern Med. 2008;23(12):2053-7.
King HB, Battles J, Baker DP, Alonso A, Salas E, Webster J, et al. TeamSTEPPS: team strategies and tools to enhance performance and patient safety. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008.
Weaver SJ, Lubomksi LH, Wilson RF, Pfoh ER, Martinez KA, Dy SM. Promoting a culture of safety as a patient safety strategy. Ann Intern Med. 2016;158(5 Pt 2):369-74.
Camacho-Rodríguez DE, Carrasquilla-Baza DA, Dominguez-Cancino KA, Palmieri PA. Patient safety culture in Latin American hospitals: a systematic review with meta-analysis. Int J Environ Res Public Health. 2022;19(21):14380.
Azami-Aghdash S, Ebadifard Azar F, Rezapour A, Azami A, Rasi V, Klvany K. Patient safety culture in hospitals of Iran: a systematic review and meta-analysis. Med J Islam Repub Iran. 2015;29:251.
Olsen E, Leonardsen ACL. Use of the Hospital Survey of Patient Safety Culture in Norwegian hospitals: a systematic review. Int J Environ Res Public Health. 2021;18(12):6518.
Blazin LJ, Sitthi-Amorn J, Hoffman JM, Burlison JD. Improving patient handoffs and transitions through adaptation and implementation of I-PASS across multiple handoff settings. Pediatr Qual Saf. 2020;5(4):e323.
American College of Obstetricians and Gynecologists. Communication strategies for patient handoffs. Available from: https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2012/02/communication-strategies-for-patient-handoffs.
Brattebø G, Flaatten HK. Errors in medicine: punishment versus learning medical adverse events revisited – expanding the frame. Curr Opin Anaesthesiol. 2023.
Wiese A, Bennett D. Orientation of medical trainees to a new clinical environment (the ready-steady-go model): a constructivist grounded theory study. BMC Med Educ. 2022;22(1).
Rahmani M. Medical trainees and the Dunning–Kruger effect: when they don’t know what they don’t know. J Grad Med Educ. 2020;12(5):532-4.
Doyen B, Vlerick P, Maertens H, Vermassen F, Van Herzeele I. Non-technical attributes and surgical experience: a cross-sectional study comparing communication styles and attitudes in surgical staff, trainees and applicants. Int J Surg. 2019;63:83-9.
de Lima Garcia C, Bezerra IMP, Ramos JLS, do Valle JETMR, Bezerra de Oliveira ML, Abreu LC. Association between culture of patient safety and burnout in pediatric hospitals. PLoS One. 2019;14(6):e0218756.
Profit J, Sharek PJ, Amspoker AB, Kowalkowski MA, Nisbet CC, Thomas EJ, et al. Burnout in the NICU setting and its relation to safety culture. BMJ Qual Saf. 2014;23(10):806-13.
Welp A, Meier LL, Manser T. Emotional exhaustion and workload predict clinician-rated and objective patient safety. Front Psychol. 2015;5:1573.
Granel N, Manresa-Domínguez JM, Watson CE, Gómez-Ibáñez R, Bernabeu-Tamayo MD. Nurses’ perceptions of patient safety culture: a mixed-methods study. BMC Health Serv Res. 2020;20(1).
Kakemam E, Gharaee H, Rajabi MR, Nadernejad M, Khakdel Z, Raeissi P, et al. Nurses’ perception of patient safety culture and its relationship with adverse events: a national questionnaire survey in Iran. BMC Nurs. 2021;20(1).
Published
How to Cite
License
Copyright (c) 2024 Ganesh Chilukuri, Thomas Westerman

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- The Author retains copyright in the Work, where the term “Work” shall include all digital objects that may result in subsequent electronic publication or distribution.
- Upon acceptance of the Work, the author shall grant to the Publisher the right of first publication of the Work.
- The Author shall grant to the Publisher and its agents the nonexclusive perpetual right and license to publish, archive, and make accessible the Work in whole or in part in all forms of media now or hereafter known under a Creative Commons Attribution 4.0 International License or its equivalent, which, for the avoidance of doubt, allows others to copy, distribute, and transmit the Work under the following conditions:
- Attribution—other users must attribute the Work in the manner specified by the author as indicated on the journal Web site; with the understanding that the above condition can be waived with permission from the Author and that where the Work or any of its elements is in the public domain under applicable law, that status is in no way affected by the license.
- The Author is able to enter into separate, additional contractual arrangements for the nonexclusive distribution of the journal's published version of the Work (e.g., post it to an institutional repository or publish it in a book), as long as there is provided in the document an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post online a prepublication manuscript (but not the Publisher’s final formatted PDF version of the Work) in institutional repositories or on their Websites prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. Any such posting made before acceptance and publication of the Work shall be updated upon publication to include a reference to the Publisher-assigned DOI (Digital Object Identifier) and a link to the online abstract for the final published Work in the Journal.
- Upon Publisher’s request, the Author agrees to furnish promptly to Publisher, at the Author’s own expense, written evidence of the permissions, licenses, and consents for use of third-party material included within the Work, except as determined by Publisher to be covered by the principles of Fair Use.
- The Author represents and warrants that:
- the Work is the Author’s original work;
- the Author has not transferred, and will not transfer, exclusive rights in the Work to any third party;
- the Work is not pending review or under consideration by another publisher;
- the Work has not previously been published;
- the Work contains no misrepresentation or infringement of the Work or property of other authors or third parties; and
- the Work contains no libel, invasion of privacy, or other unlawful matter.
- The Author agrees to indemnify and hold Publisher harmless from the Author’s breach of the representations and warranties contained in Paragraph 6 above, as well as any claim or proceeding relating to Publisher’s use and publication of any content contained in the Work, including third-party content.
Enforcement of copyright
The IJMS takes the protection of copyright very seriously.
If the IJMS discovers that you have used its copyright materials in contravention of the license above, the IJMS may bring legal proceedings against you seeking reparation and an injunction to stop you using those materials. You could also be ordered to pay legal costs.
If you become aware of any use of the IJMS' copyright materials that contravenes or may contravene the license above, please report this by email to contact@ijms.org
Infringing material
If you become aware of any material on the website that you believe infringes your or any other person's copyright, please report this by email to contact@ijms.org