From Hope to Hardship: Understanding the Impact of Hierarchies and Violence in Medicine
DOI:
https://doi.org/10.5195/ijms.2024.2679Keywords:
Medical Students, Medical Education, Workplace Violence, Hierarchies, Health Personnel, Medical Hierarchies, Burnout, Psychological Safety, Mistreatment in Medicine, Systemic Change, Bullying and Harassment, Trainee Well-being, Medical Education Culture, Leadership and AdvocacyAbstract
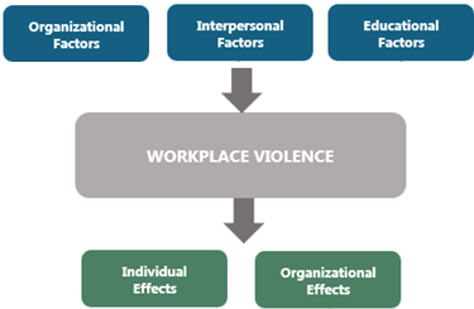
This article is an experience piece reflecting on my journey through medical school rotations, highlighting the pervasive nature of workplace violence (WPV) and its impact on students' motivation and mental health. I discuss the high incidence of mistreatment and its correlation with burnout, imposter syndrome, and decreased academic performance among trainees. I emphasize the importance of recognizing and addressing subtle forms of WPV, including microaggressions and systemic issues, and advocate for proactive measures such as education, training, and fostering cultural change within healthcare institutions. Through reflecting on my experiences and observations, I aim to inspire systemic change and empower individuals to contribute to a healthier, more empathetic medical culture.
References
Occupational Health and Safety Administration. Workplace Violence. Available from: https://www.osha.gov/hospitals/workplace-violence. Cited May 1, 2024.
Hershkovitz MS, Turner N, Barling J, Arnold KA, Dupré KE, Inness M, et al. Predicting workplace aggression: a meta-analysis. J Appl Psychol. 2007;92(1):228-238.
Escribano RB, Beneit J, Luis Garcia J. Violence in the workplace: some critical issues looking at the health sector. Heliyon. 2019;5(3):e01283.
Hamui-Sutton L, Paz-Rodriguez F, Sánchez-Guzmán A, Vives-Varela T, Corona T. Violence and Clinical Learning Environments in Medical Residencies. Int J Environ Res Public Health. 2023;20(18):6754.
Markman JD, Soeprono TM, Combs HL, Cosgrove EM. Medical student mistreatment: understanding 'public humiliation'. Med Educ Online. 2019;24(1):1615367.
Scott KM, Caldwell PH, Barnes EH, Barrett J. "Teaching by humiliation" and mistreatment of medical students in clinical rotations: a pilot study. Med J Aust. 2015;203(4):185e.1-185e.6.
Vanstone M, Grierson L. Thinking about social power and hierarchy in medical education. Med Educ. 2022;56(1):91-97.
Salehi PP, Jacobs D, Suhail-Sindhu T, Judson BL, Azizzadeh B, Lee YH, et al. Consequences of Medical Hierarchy on Medical Students, Residents, and Medical Education in Otolaryngology. Otolaryngol Head Neck Surg. 2020;163(5):906-914.
Essex R, Kennedy J, Miller D, Jameson J. A scoping review exploring the impact and negotiation of hierarchy in healthcare organisations. Nurs Inq. 2023;30(4):e12571.
Rajakumar HK, Gãman MA, Puyana JC, Bonilla-Escobar FJ. Transforming Toxic Research Cultures: Protecting the Future of Medical Students and Early Career Researchers – Part I. Int J Med Stud. 2024;12(2):128–132.
Norman S. The Shame Is Not Mine: Addressing Abuse of Power Dynamics in Medical Training. Int J Med Stud. 2024;12(3):354-365.
Yan, W., Bao, N., Zheng, S., Wang, H., Yue, D., & Chen, L. (2023). The impacts of patient mistreatment on healthcare workers' role behaviors: a study in Chinese Fangcang shelter hospitals. BMC nursing, 22(1), 444.
Legassie J, Zibrowski EM, Goldszmidt MA. Measuring resident well-being: impostorism and burnout syndrome in residency. J Gen Intern Med. 2008;23(7):1090-1094.
Rosenberg DA. Medical student abuse. An unnecessary and preventable cause of stress. JAMA. 1984;251(6):739-742.
Barbanti PCM, Oliveira SRL, de Medeiros AE, Bitencourt MR, Victorino SVZ, Bitencourt MR, et al. Prevalence and Impact of Academic Violence in Medical Education. Int J Environ Res Public Health. 2022;19(18):11519.
Timm A. 'It would not be tolerated in any other profession except medicine': survey reporting on undergraduates' exposure to bullying and harassment in their first placement year. BMJ Open. 2014;4(7):e005140.
Caruso R, Toffanin T, Folesani F, Biancosino B, Romagnolo F, Riba MB, et al. Violence Against Physicians in the Workplace: Trends, Causes, Consequences, and Strategies for Intervention. Curr Psychiatry Rep. 2022 Dec;24(12):911-924.
National Institute for Occupational Safety and Health. (2006). Workplace violence prevention strategies and research needs : report from the conference Partnering in Workplace Violence Prevention: Translating Research to Practice, November 15-17, 2004, Baltimore, Maryland.
Arnetz JE. The Joint Commission's New and Revised Workplace Violence Prevention Standards for Hospitals: A Major Step Forward Toward Improved Quality and Safety. Jt Comm J Qual Patient Saf. 2022 Apr;48(4):241-245.
Jones CB, Sousane Z, Mossburg S. Addressing Workplace Violence and Creating a Safer Workplace. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2023.
Einarsen SH, Notelaers G. Measuring exposure to bullying at work: validity, factor structure and psychometric properties of the Negative Acts Questionnaire-Revised. Work Stress. 2009;23(1):24-44.
Taylor R. Nurses' perceptions of horizontal violence. Glob Qual Nurs Res. 2016;3:2333393616641002.
Yosep I, Mardhiyah A, Hendrawati H, Hendrawati S. Interventions for reducing negative impacts of workplace violence among health workers: a scoping review. J Multidiscip Healthc. 2023;16:1409-1421
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2024 Ximena Cors Cepeda

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- The Author retains copyright in the Work, where the term “Work” shall include all digital objects that may result in subsequent electronic publication or distribution.
- Upon acceptance of the Work, the author shall grant to the Publisher the right of first publication of the Work.
- The Author shall grant to the Publisher and its agents the nonexclusive perpetual right and license to publish, archive, and make accessible the Work in whole or in part in all forms of media now or hereafter known under a Creative Commons Attribution 4.0 International License or its equivalent, which, for the avoidance of doubt, allows others to copy, distribute, and transmit the Work under the following conditions:
- Attribution—other users must attribute the Work in the manner specified by the author as indicated on the journal Web site; with the understanding that the above condition can be waived with permission from the Author and that where the Work or any of its elements is in the public domain under applicable law, that status is in no way affected by the license.
- The Author is able to enter into separate, additional contractual arrangements for the nonexclusive distribution of the journal's published version of the Work (e.g., post it to an institutional repository or publish it in a book), as long as there is provided in the document an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post online a prepublication manuscript (but not the Publisher’s final formatted PDF version of the Work) in institutional repositories or on their Websites prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. Any such posting made before acceptance and publication of the Work shall be updated upon publication to include a reference to the Publisher-assigned DOI (Digital Object Identifier) and a link to the online abstract for the final published Work in the Journal.
- Upon Publisher’s request, the Author agrees to furnish promptly to Publisher, at the Author’s own expense, written evidence of the permissions, licenses, and consents for use of third-party material included within the Work, except as determined by Publisher to be covered by the principles of Fair Use.
- The Author represents and warrants that:
- the Work is the Author’s original work;
- the Author has not transferred, and will not transfer, exclusive rights in the Work to any third party;
- the Work is not pending review or under consideration by another publisher;
- the Work has not previously been published;
- the Work contains no misrepresentation or infringement of the Work or property of other authors or third parties; and
- the Work contains no libel, invasion of privacy, or other unlawful matter.
- The Author agrees to indemnify and hold Publisher harmless from the Author’s breach of the representations and warranties contained in Paragraph 6 above, as well as any claim or proceeding relating to Publisher’s use and publication of any content contained in the Work, including third-party content.
Enforcement of copyright
The IJMS takes the protection of copyright very seriously.
If the IJMS discovers that you have used its copyright materials in contravention of the license above, the IJMS may bring legal proceedings against you seeking reparation and an injunction to stop you using those materials. You could also be ordered to pay legal costs.
If you become aware of any use of the IJMS' copyright materials that contravenes or may contravene the license above, please report this by email to contact@ijms.org
Infringing material
If you become aware of any material on the website that you believe infringes your or any other person's copyright, please report this by email to contact@ijms.org