From Student to Physician: Determining Which Lifestyle Behaviors May Be Risk Factors for Burnout at a South Florida Medical School
DOI:
https://doi.org/10.5195/ijms.2023.2022Keywords:
Students, Burnout, Professional, Risk reduction behavior, Support, Social, Medical student, MD, MBBS, MD-PhD, MD-MSc, DO, Lifestyle, Healthy lifestyle, Behavior, United States, Florida, Professional Burnout, Occupational Burnout, Career Burnout, Stress, Psychiatry, Psychology, MD student, MBBS student, MD-MSc student, MD-PhD studentAbstract
Background: Compared to other professions, physicians have significantly higher rates of burnout and poor lifestyle behaviors, including inadequate sleep, poor diet, limited exercise, and lack of supportive social relationships. Among physicians in training, burnout and increasingly poor lifestyle behaviors can begin as early as the preclinical years of medical school.
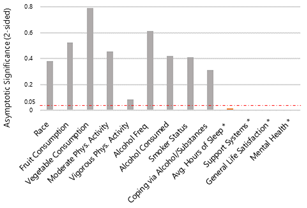
Methods: A cross-sectional survey composed of questions from standardized surveys measuring diet (Yaroch’s FVS), exercise (NPAQ-S), sleep (NHANES), stress management (HRQOL), social support (BRFSS), substance use (AUDIT-QF, WHO), and burnout (Mini-Z) was conducted on a South Florida medical school in May 2021. One hundred forty-four students fully completed the survey for a response rate of 16%. Descriptive analysis was performed via SPSS to determine the effects of these lifestyle factors on the likelihood of student burnout.
Results: In this sample of medical students, over half (61%) experienced burnout per the Single Item Burnout Measure. Independently, lack of sleep (p<0.02) and decreased social support (p<0.001) were lifestyle factors positively associated with increased risk of burnout. Furthermore, students who experienced burnout reported more poor mental health days and decreased life satisfaction (p<0.001).
Conclusion: Over half of the medical students experienced burnout. Lack of sleep and lack of social support were significantly associated with increased risk of burnout. In addition, burned-out students showed significantly increased levels of poor mental health and decreased life satisfaction. These findings help us identify specific lifestyle factors that institutions could use to further combat medical student burnout.
References
De Hert S. Burnout in Healthcare Workers: Prevalence, Impact and Preventative Strategies. Local Reg Anesth. 2020;13:171-83. DOI: https://doi.org/10.2147/LRA.S240564
Tawfik DS, Profit J, Morgenthaler TI, Satele DV, Sinsky CA, Dyrbye LN, et al. Physician Burnout, Well-being, and Work Unit Safety Grades in Relationship to Reported Medical Errors. Mayo Clin Proc. 2018;93(11):1571-80. DOI: https://doi.org/10.1016/j.mayocp.2018.05.014
Wiskar K. Physician health: A review of lifestyle behaviors and preventive health care among physicians. British Columbia Medical Journal. 2012;54(8):419–23.
DiMatteo MR, Sherbourne CD, Hays RD, Ordway L, Kravitz RL, McGlynn EA, et al. Physicians' characteristics influence patients' adherence to medical treatment: results from the Medical Outcomes Study. Health Psychol. 1993;12(2):93-102. DOI: https://doi.org/10.1037/0278-6133.12.2.93
Cecil J, McHale C, Hart J, Laidlaw A. Behaviour and burnout in medical students. Med Educ Online. 2014;19:25209. DOI: https://doi.org/10.3402/meo.v19.25209
Ishak W, Nikravesh R, Lederer S, Perry R, Ogunyemi D, Bernstein C. Burnout in medical students: a systematic review. Clin Teach. 2013;10(4):242-5. DOI: https://doi.org/10.1111/tct.12014
Dyrbye LN, Satele D, West CP. Association of Characteristics of the Learning Environment and US Medical Student Burnout, Empathy, and Career Regret. JAMA Netw Open. 2021 Aug 2;4(8):e2119110. doi: 10.1001/jamanetworkopen.2021.19110. DOI: https://doi.org/10.1001/jamanetworkopen.2021.19110
Jackson ER, Shanafelt TD, Hasan O, Satele DV, Dyrbye LN. Burnout and Alcohol Abuse/Dependence Among U.S. Medical Students. Acad Med. 2016;91(9):1251-6. DOI: https://doi.org/10.1097/ACM.0000000000001138
Wolf MR, Rosenstock JB. Inadequate Sleep and Exercise Associated with Burnout and Depression Among Medical Students. Acad Psychiatry. 2017;41(2):174-9. DOI: https://doi.org/10.1007/s40596-016-0526-y
Mazurkiewicz R, Korenstein D, Fallar R, Ripp J. The prevalence and correlations of medical student burnout in the pre-clinical years: A cross-sectional study. Psychology, Health & Medicine. 2012;17(2):188–95. DOI: https://doi.org/10.1080/13548506.2011.597770
Yaroch AL, Tooze J, Thompson FE, Blanck HM, Thompson OM, Colón-Ramos U, et al. Evaluation of three short dietary instruments to assess fruit and vegetable intake: The National Cancer Institute's Food Attitudes and Behaviors Survey. Journal of the Academy of Nutrition and Dietetics. 2012;112(10):1570–7. DOI: https://doi.org/10.1016/j.jand.2012.06.002
Danquah IH, Petersen CB, Skov SS, Tolstrup JS. Validation of the NPAQ-short – a brief questionnaire to monitor physical activity and compliance with the WHO recommendations. BMC Public Health. 2018;18(1). DOI: https://doi.org/10.1186/s12889-018-5538-y
Kaarne T, Aalto M, Kuokkanen M, Seppä K. Audit-C, audit-3 and audit-QF in screening risky drinking among Finnish occupational health-care patients. Drug and Alcohol Review. 2010;29(5):563–7. DOI: https://doi.org/10.1111/j.1465-3362.2010.00172.x
Rohland BM, Kruse GR, Rohrer JE. Validation of a single-item measure of burnout against the Maslach Burnout Inventory Among Physicians. Stress and Health. 2004;20(2):75–9. DOI: https://doi.org/10.1002/smi.1002
Dolan ED, Mohr D, Lempa M, Joos S, Fihn SD, Nelson KM, et al. Using a single item to measure burnout in primary care staff: a psychometric evaluation. J Gen Intern Med. 2015 May;30(5):582-7. doi: 10.1007/s11606-014-3112-6. Epub 2014 Dec 2. PMID: 25451989; PMCID: PMC4395610. DOI: https://doi.org/10.1007/s11606-014-3112-6
Lianov L, Johnson M. Physician competencies for prescribing lifestyle medicine. JAMA. 2010 Jul 14;304(2):202-3. DOI: https://doi.org/10.1001/jama.2010.903
Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, et al. Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015 Jun 1;38(6):843-4. DOI: https://doi.org/10.5665/sleep.4716
Azad MC, Fraser K, Rumana N, Abdullah AF, Shahana N, Hanly PJ, et al. Sleep disturbances among medical students: a global perspective. J Clin Sleep Med. 2015 Jan 15;11(1):69-74. DOI: https://doi.org/10.5664/jcsm.4370
Pew Research Center. How Americans feel about the satisfactions and stresses of Modern Life. Available from: https://www.pewresearch.org/fact-tank/2020/02/05/how-americans-feel-about-the-satisfactions-and-stresses-of-modern-life/. Updated Feb 5; 2020; cited Jan 9,2022.
Youssef FF. Medical student stress, Burnout and depression in Trinidad and Tobago. Academic Psychiatry. 2016;40(1):69–75. DOI: https://doi.org/10.1007/s40596-015-0468-9
Jeong Y, Kim JY, Ryu JS, Lee KE, Ha EH, Park H. The Associations between Social Support, Health-Related Behaviors, Socioeconomic Status and Depression in Medical Students. Epidemiol Health. 2010;32:e2010009. DOI: https://doi.org/10.4178/epih/e2010009
Yamada Y, Klugar M, Ivanova K, Oborna I. Psychological distress and academic self-perception among international medical students: the role of peer social support. BMC Med Educ. 2014;14:256. DOI: https://doi.org/10.1186/s12909-014-0256-3
Dyrbye LN, Thomas MR, Huntington JL, Lawson KL, Novotny PJ, Sloan JA, et al. Personal life events and medical student burnout: a multicenter study. Acad Med. 2006;81(4):374-84. DOI: https://doi.org/10.1097/00001888-200604000-00010
Pantell M, Rehkopf D, Jutte D, Syme SL, Balmes J, Adler N. Social isolation: a predictor of mortality comparable to traditional clinical risk factors. Am J Public Health. 2013;103(11):2056-62. DOI: https://doi.org/10.2105/AJPH.2013.301261
Lee KP, Yeung N, Wong C, Yip B, Luk LHF, Wong S. Prevalence of medical students' burnout and its associated demographics and lifestyle factors in Hong Kong. PLoS One. 2020;15(7):e0235154. DOI: https://doi.org/10.1371/journal.pone.0235154
West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388(10057):2272-81. DOI: https://doi.org/10.1016/S0140-6736(16)31279-X
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2023 Rachel Lin, Heather Woolery-Lloyd, BreAnne Young, Sonjia Kenya

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- The Author retains copyright in the Work, where the term “Work” shall include all digital objects that may result in subsequent electronic publication or distribution.
- Upon acceptance of the Work, the author shall grant to the Publisher the right of first publication of the Work.
- The Author shall grant to the Publisher and its agents the nonexclusive perpetual right and license to publish, archive, and make accessible the Work in whole or in part in all forms of media now or hereafter known under a Creative Commons Attribution 4.0 International License or its equivalent, which, for the avoidance of doubt, allows others to copy, distribute, and transmit the Work under the following conditions:
- Attribution—other users must attribute the Work in the manner specified by the author as indicated on the journal Web site; with the understanding that the above condition can be waived with permission from the Author and that where the Work or any of its elements is in the public domain under applicable law, that status is in no way affected by the license.
- The Author is able to enter into separate, additional contractual arrangements for the nonexclusive distribution of the journal's published version of the Work (e.g., post it to an institutional repository or publish it in a book), as long as there is provided in the document an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post online a prepublication manuscript (but not the Publisher’s final formatted PDF version of the Work) in institutional repositories or on their Websites prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. Any such posting made before acceptance and publication of the Work shall be updated upon publication to include a reference to the Publisher-assigned DOI (Digital Object Identifier) and a link to the online abstract for the final published Work in the Journal.
- Upon Publisher’s request, the Author agrees to furnish promptly to Publisher, at the Author’s own expense, written evidence of the permissions, licenses, and consents for use of third-party material included within the Work, except as determined by Publisher to be covered by the principles of Fair Use.
- The Author represents and warrants that:
- the Work is the Author’s original work;
- the Author has not transferred, and will not transfer, exclusive rights in the Work to any third party;
- the Work is not pending review or under consideration by another publisher;
- the Work has not previously been published;
- the Work contains no misrepresentation or infringement of the Work or property of other authors or third parties; and
- the Work contains no libel, invasion of privacy, or other unlawful matter.
- The Author agrees to indemnify and hold Publisher harmless from the Author’s breach of the representations and warranties contained in Paragraph 6 above, as well as any claim or proceeding relating to Publisher’s use and publication of any content contained in the Work, including third-party content.
Enforcement of copyright
The IJMS takes the protection of copyright very seriously.
If the IJMS discovers that you have used its copyright materials in contravention of the license above, the IJMS may bring legal proceedings against you seeking reparation and an injunction to stop you using those materials. You could also be ordered to pay legal costs.
If you become aware of any use of the IJMS' copyright materials that contravenes or may contravene the license above, please report this by email to contact@ijms.org
Infringing material
If you become aware of any material on the website that you believe infringes your or any other person's copyright, please report this by email to contact@ijms.org







