Assessment of Antimicrobial Resistance and Susceptibility Pattern of UTI-causing Microorganisms in Southern Punjab, Pakistan
DOI:
https://doi.org/10.5195/ijms.2024.2163Keywords:
Urinary tract infection , Antibiotic Resistance, Drug Resistance, Bacterial, Antimicrobial Resistance, Uropathogens, Southern Punjab, Antibiotic Susceptibility, Urinary Tract Infections (UTIs), Escherichia Coli, Kirby Bauer Test, Imipenem Sensitivity, Multidrug Resistance, Clinical MicrobiologyAbstract
Background: Bacterial resistance against antibiotics has become a global challenge and measures are needed to stop this. The aim of this study is to highlight this problem and to determine the antibiotic susceptibility pattern of organisms in Southern Punjab, Pakistan.
Method: This descriptive cross-sectional study was conducted in Sheikh Zayed Medical Hospital, Rahim Yar Khan. The urine samples obtained from 4 different wards were sent for culture and sensitivity analysis. 9 antibiotics (Nitrofurantoin, Fosfomycin, Ciprofloxacin, Ceftriaxone, Trimethoprim-Sulfamethoxazole, Norfloxacin, Linezolid, Amoxicillin, and Imipenem) were tested against 5 isolated strains of uropathogens using Kirby Bauer disk diffusion test. The sensitivity reports were obtained, and data points were entered into a spreadsheet and analysed using SPSS.
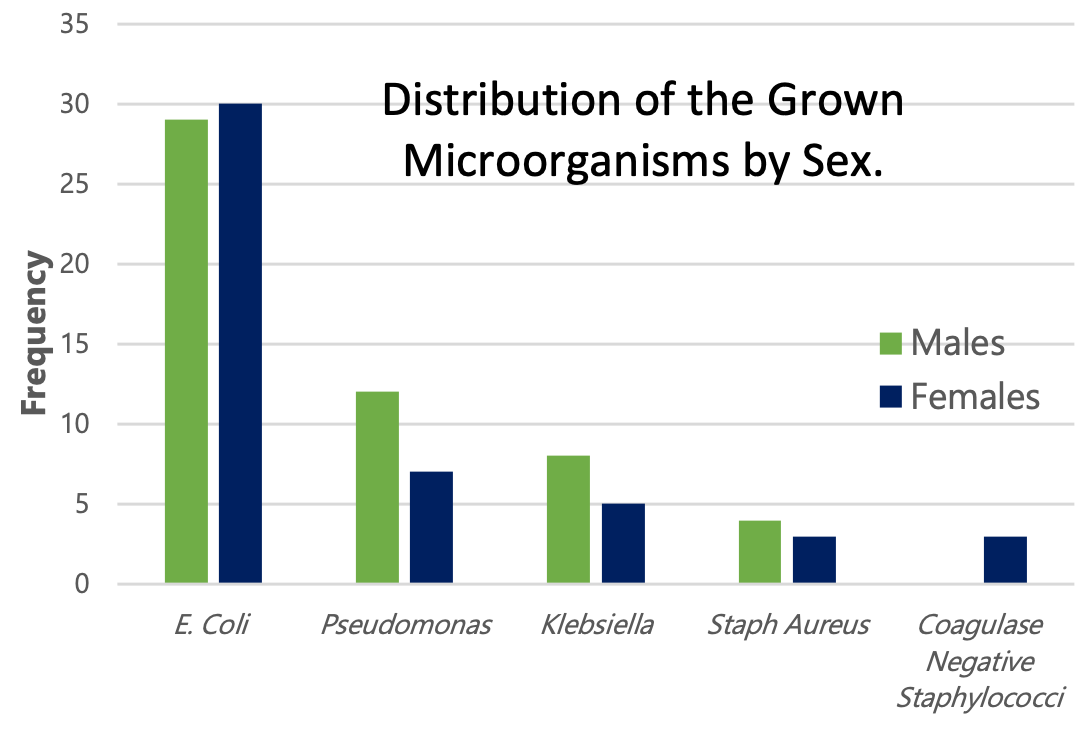
Results: Out of 101 samples of uropathogens that showed positive growths (42.08%), 53 (52.4%) were from male patients and 48 (47.5%) positive growths were from females. Escherichia Coli had the highest positive growths (58%) followed by Pseudomonas (19%) Klebsiella (13%), Staphylococcus Aureus (7%) and Coagulase-negative staphylococci (3%). Imipenem was the most sensitive drug whereas the highest resistance by organisms was developed against TMP-SMX. No significant association(p>0.05) was found between any of the anti-microbial drugs and Escherichia coli, gram-positive uropathogens, and gram negative uropathogens.
Conclusion: The high increasing rate of broad-spectrum antibiotics resistance suggests that diagnostic and culture tests should be encouraged in hospitals. Based on these test results, appropriate antibiotics should be prescribed. The limitations include the inability to distinguish between nosocomial and community-acquired urinary tract infections and also did not consider other demographic factors like age.
References
Sulis G, Adam P, Nafade V, Gore G, Daniels B, Daftary A, et al. Antibiotic prescription practices in primary care in low- and middle-income countries: A systematic review and meta-analysis. PLoS Med. 2020;17(6):e1003139.
Abdelrazik E, El-Hadidi M. Tracking Antibiotic Resistance from the Environment to Human Health. Methods Mol Biol. 2023;2649:289–301.
Bilal H, Khan MN, Rehman T, Hameed MF, Yang X. Antibiotic resistance in Pakistan: a systematic review of past decade. BMC Infect Dis. 2021;21(1):244.
Ul Mustafa Z, Salman M, Aldeyab M, Kow CS, Hasan SS. Antimicrobial consumption among hospitalized patients with COVID-19 in Pakistan. SN Compr Clin Med. 2021;3(8):1691–5.
Muzammil M, Adnan M, Sikandar SM, Waheed MU, Javed N, Ur Rehman MF. Study of culture and sensitivity patterns of urinary tract infections in patients presenting with urinary symptoms in a tertiary care hospital. Cureus. 2020;12(2):e7013.
Alemkere G, Tenna A, Engidawork E. Antibiotic use practice and predictors of hospital outcome among patients with systemic bacterial infection: Identifying targets for antibiotic and health care resource stewardship. PLoS One. 2019;14(2):e0212661.
Tamadonfar KO, Omattage NS, Spaulding CN, Hultgren SJ. Reaching the end of the line: Urinary tract infections. Microbiol Spectr. 2019;7(3).
Kot B. Antibiotic Resistance Among Uropathogenic Escherichia coli. Pol J Microbiol. 2019;68(4):403–15.
Sante L, Lecuona M, Jaime-Aguirre A, Arias A. Risk factors to secondary nosocomial bacteremia to UTI in a tertiary hospital. Rev Esp Quimioter. 2019;32(4):311–6.
Kranz J, Schmidt S, Wagenlehner Florian and Schneidewind L. Catheter-associated urinary tract infections in adult patients. Dtsch Arztebl Int. 2020;117(6):83–8.
Karlowsky JA, Lob SH, Kazmierczak KM, Young K, Motyl MR, Sahm DF. In vitro activity of imipenem/relebactam against Enterobacteriaceae and Pseudomonas aeruginosa isolated from intraabdominal and urinary tract infection samples: SMART Surveillance United States 2015-2017. J Glob Antimicrob Resist. 2020;21:223–8.
Ravishankar U, P S, Thayanidhi P. Antimicrobial resistance among uropathogens: Surveillance report from south India. Cureus. 2021;13(1):e12913.
Chao YS, Farrah K. Fluoroquinolones for the Treatment of Urinary Tract Infection: A Review of Clinical Effectiveness, Cost-Effectiveness, and Guidelines. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health; 2019.
Ten Doesschate T, Kuiper S, van Nieuwkoop Cees and Hassing RJ, Ketels T, van Mens Suzan P and van den Bijllaardt W, van der Bij AK, et al. Fosfomycin vs ciprofloxacin as oral step-down treatment for Escherichia coli febrile urinary tract infections in women: A randomized, placebo-controlled, double-blind, multicenter trial. Clin Infect Dis. 2022;75(2):221–9.
Miyoshi-Akiyama T, Tada T, Ohmagari N, Viet Hung N, Tharavichitkul P, Pokhrel BM, et al. Emergence and Spread of Epidemic Multidrug-Resistant Pseudomonas aeruginosa. Genome Biol Evol. 2017;9(12):3238–45.
Majumder MAA, Rahman S, Cohall Damian and Bharatha A, Singh K, Haque M, Gittens-St Hilaire M. Antimicrobial stewardship: Fighting antimicrobial resistance and protecting global public health. Infect Drug Resist. 2020;13:4713–38.
Redfern J, Bowater L, Coulthwaite L, Verran J. Raising awareness of antimicrobial resistance among the general public in the UK: the role of public engagement activities. JAC Antimicrob Resist. 2020;2(1):dlaa012.
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2024 Muhammad Mehwar Anjum; Faiza Khalid; Rida Saleem, Muhammad Awais Bin Abdul Malik, Muhammad Rizwan

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- The Author retains copyright in the Work, where the term “Work” shall include all digital objects that may result in subsequent electronic publication or distribution.
- Upon acceptance of the Work, the author shall grant to the Publisher the right of first publication of the Work.
- The Author shall grant to the Publisher and its agents the nonexclusive perpetual right and license to publish, archive, and make accessible the Work in whole or in part in all forms of media now or hereafter known under a Creative Commons Attribution 4.0 International License or its equivalent, which, for the avoidance of doubt, allows others to copy, distribute, and transmit the Work under the following conditions:
- Attribution—other users must attribute the Work in the manner specified by the author as indicated on the journal Web site; with the understanding that the above condition can be waived with permission from the Author and that where the Work or any of its elements is in the public domain under applicable law, that status is in no way affected by the license.
- The Author is able to enter into separate, additional contractual arrangements for the nonexclusive distribution of the journal's published version of the Work (e.g., post it to an institutional repository or publish it in a book), as long as there is provided in the document an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post online a prepublication manuscript (but not the Publisher’s final formatted PDF version of the Work) in institutional repositories or on their Websites prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. Any such posting made before acceptance and publication of the Work shall be updated upon publication to include a reference to the Publisher-assigned DOI (Digital Object Identifier) and a link to the online abstract for the final published Work in the Journal.
- Upon Publisher’s request, the Author agrees to furnish promptly to Publisher, at the Author’s own expense, written evidence of the permissions, licenses, and consents for use of third-party material included within the Work, except as determined by Publisher to be covered by the principles of Fair Use.
- The Author represents and warrants that:
- the Work is the Author’s original work;
- the Author has not transferred, and will not transfer, exclusive rights in the Work to any third party;
- the Work is not pending review or under consideration by another publisher;
- the Work has not previously been published;
- the Work contains no misrepresentation or infringement of the Work or property of other authors or third parties; and
- the Work contains no libel, invasion of privacy, or other unlawful matter.
- The Author agrees to indemnify and hold Publisher harmless from the Author’s breach of the representations and warranties contained in Paragraph 6 above, as well as any claim or proceeding relating to Publisher’s use and publication of any content contained in the Work, including third-party content.
Enforcement of copyright
The IJMS takes the protection of copyright very seriously.
If the IJMS discovers that you have used its copyright materials in contravention of the license above, the IJMS may bring legal proceedings against you seeking reparation and an injunction to stop you using those materials. You could also be ordered to pay legal costs.
If you become aware of any use of the IJMS' copyright materials that contravenes or may contravene the license above, please report this by email to contact@ijms.org
Infringing material
If you become aware of any material on the website that you believe infringes your or any other person's copyright, please report this by email to contact@ijms.org