Medical Students’ Study Habits Through a Sociocultural Lens: A Systematic Literature Review
DOI:
https://doi.org/10.5195/ijms.2024.2200Keywords:
Sociology of Medicine, Habits, Self-Directed Learning as Topic, State of the Art Review, Study Habits, Sociocultural Factors, Medical Students, Systematic Review, Learning Strategies, Academic Performance, Socioeconomic Factors, Educational Status, Health Knowledge, Attitudes, Practice, Social Support, Self Efficacy, Learning, Educational Measurement, Cognitive Processes, Educational Technology, Social Learning, Student Behavior, Health Promotion, Psychological Theory, CurriculumAbstract
This study investigates the literature on medical students' study habits and the surrounding sociocultural factors. A systematic literature review was undertaken, aiming to establish what is known, identify gaps in the literature and suggest what further research needs to be done. The review followed the PRISMA guidelines and identified 13 papers that were within the inclusion criteria. These papers were analyzed and discussed through a sociocultural lens, dividing the results into four sociocultural groupings: Personal, Behavioral, Environmental and Cognitive. The findings suggest that while sociocultural factors influence medical students' study habits, individual behaviors and attitudes predominantly guide their study decisions. The findings also suggest that there is little research into the intersection of these factors. It is recommended that the factors drawn from this systematic review be used to formulate more direct research into study habits with a magnified approach to help provide medical institutions, policymakers, and students with information to better inform their decisions and produce efficient, healthy study habits.
References
Riemenschneider H, Balázs P, Balogh E, Bartels A, Bergmann A, Cseh K, et al. Do socio-cultural factors influence medical students' health status and health-promoting behaviors? A cross-sectional multicenter study in Germany and Hungary. BMC Public Health. 2016;16:1-10
Miller CJ. Implementation of a study skills program for entering at-risk medical students. Adv Physiol Educ. 2014;38(3):229-34.
Anwar K, Adnan M. Online learning amid the COVID-19 pandemic: Students perspectives. J Pedagog Research. 2020;1:45-51.
Walck-Shannon EM, Rowell SF, Frey RF. To what extent do study habits relate to performance? CBE—Life Sci Educ. 2021; 20(1):ar6.
Mendezabal MJ. Study habits and attitudes: The road to academic success. Open Sci Repos Educ. 2013;e70081928.
Pitan OO. Poor study habit as an educational problem among university undergraduates in the contemporary times and effective management strategies. Int J of H and Soc Sci Invention. 2013;2(11):72-6.
Ferguson E, James D, Madeley L. Factors associated with success in medical school: systematic review of the literature. BMJ. 2002;324(7343):952-7.
General Medical Council. Tomorrow’s Doctors. London. 2009:22.
General Medical Council. Outcomes for Graduates. London. 2018:28.
Wynter L, Burgess A, Kalman E, Heron JE, Bleasel J. Medical students: what educational resources are they using? BMC Med Educ. 2019;19(1):36.
Bourdieu P. The forms of capital. In The sociology of economic life. 3rd ed. Oxfordshire: Routledge. 2018:78-92.
Ahmed MI. Responding to COVID-19 via online learning: The relationship between facebook intensity, community factors with social capital and academic performance. PalArch's J Archaeology of Egypt / Egyptology. 2020;17(6):779-806.
Feltovich PJ, Spiro RJ, Coulson RL, Feltovich J. Collaboration within and among minds: Mastering complexity, individually and in groups. CSCL: Theory and practice of an emerging paradigm. Computers, cognition, and work. Hillsdale, NJ, US: Lawrence Erlbaum Associates, Inc; 1996.
Boehler ML, Schwind CJ, Folse R, Dunnington G, Markwell S, Dutta S. An evaluation of study habits of third-year medical students in a surgical clerkship. Am J Surg. 2001;181(3):268-71.
Nicholson S, Cleland JA. ‘It’s making contacts’: Notions of social capital and implications for widening access to medical education. Adv in Health Sci Educ. 2017;22(2):477-90.
Entwistle N. Improving teaching through research on student learning. University teaching: International perspectives. 1998:73-112.
Nelson IA. Starting over on campus or sustaining existing ties? Social capital during college among rural and non-rural college graduates. Qual Soc. 2019;42(1):93-116.
Harden RM, Sowden S, Dunn WR. Educational strategies in curriculum development: the SPICES model. Med Educ. 1984;18(4):284-97.
Bandura A, Walters RH. Social learning theory. Prentice Hall: Englewood cliffs. 1977.
Schunk DH. Self-efficacy and achievement behaviors. Educ Psych Review. 1989;1:173-208.
Gilavand A, Emad Y. A systematic review and meta-analysis of students’ study habits in Iranian Universities of Medical Sciences. Fam Med & Primary Care Review. 2021;23(3):363-71.
Munusamy E, Ganesan M. Meta analysis of study habits and academic achievement. Shanlax Int J Arts, Sci and Humanities. 2021;8:139-45.
Khan S, Dawar J, Yasin P, Abid S, Hussain MA, Balqias H, et al., editors. A systematic review: Correlation of study habits and academic performance of medical students. 2021.
Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13(3):141-6.
Xiao Y, Watson M. Guidance on conducting a systematic literature review. J Planning Educ and Research. 2019;39(1):93-112.
Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implementation Sci. 2010;5:1-9.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Kumar S. Study habits of undergraduate students. Int J Educ and Inform Studies. 2015;5(1):17-24.
Ayodele CS, Adebiyi DR. Study habits as influence of academic performance of student nurses of Banquet State University. Int J Nursing Sci. 2013;5(2):60-65.
Jafari H, Aghaei A, Khatony A. relationship between study habits and academic achievement in students of medical sciences in Kermanshah-Iran. Adv Med Educ Pract. 2019;10:637-43.
Alzahrani SS, Soo Park Y, Tekian A. Study habits and academic achievement among medical students: A comparison between male and female subjects. Med Teach. 2018;40:S1-S9.
Rezaie Looyeh H, Seyed Fazelpour SF, Reza Masoule S, Chehrzad MM, Kazem Nejad Leili E. The relationship between the study habits and the academic performance of medical sciences students. J Holistic Nursing and Midwifery. 2017;27(2):65-73.
Credé M, Kuncel NR. Study habits, skills, and attitudes: The third pillar supporting collegiate academic performance. Persp Psychol Sc. 2008;3(6):425-53.
Zittoun T, Baucal A. The relevance of a sociocultural perspective for understanding learning and development in older age. Learn Cult Soc Interact. 2021;28:100453.
Phan HP, editor. A sociocultural perspective of learning: Developing a new theoretical tenet. 2012.
Vygotsky LS. Mind in Society: The development of higher psychological processes. Cambridge: MA: Harvard University Press. 1978.
Ahtisham Y, Parveen A. Five tips for developing useful literature summary tables for writing review articles. Evidence Based Nursing. 2021;24(2):32-34.
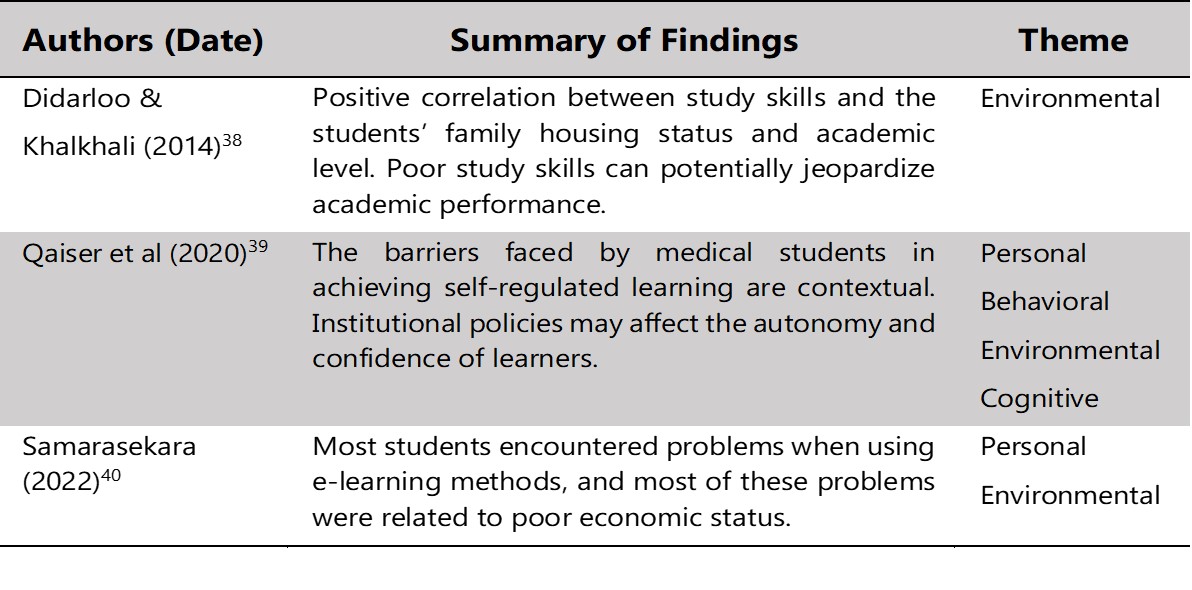
Didarloo A, Khalkhali HR. Assessing study skills among university students: an Iranian survey. J Educ Eval Health Prof. 2014;11:1-8.
Qaiser A, Waqqar S, Noor AA, Zakaria M, Iqbal F. Barriers faced by undergraduate medical students to become self-regulated learner. Pakistan J Med and Health Sci. 2020;14(4):1297-1300.
Samarasekara K. e-Learning in medical education in Sri Lanka: Survey of medical undergraduates and new graduates. JMIR Med Educ. 2022;8(1):e22096.
Jouhari Z, Haghani F, Changiz T. Factors affecting self-regulated learning in medical students: A qualitative study. Med Educ Online. 2015;28694
Shukri AK, Mubarak AS. Factors of academic success among undergraduate medical students in Taif University, Saudi Arabia: A cross-sectional study. Int J Pharm Res Allied Sci. 2019;8(1):158-70.
Jiang QX, Horta H, Yuen M. International medical students' perspectives on factors affecting their academic success in China: a qualitative study. BMC Med Educ. 2022;22(1):1-16.
Amin Z, Tani M, Eng KH, Samarasekara DD, Huak CY. Motivation, study habits, and expectations of medical students in Singapore. Med Teach. 2009;31(12):E560-E9.
Henning MA, Krägeloh C, Thompson A, Sisley R, Doherty I, Hawken SJ. Religious affiliation, quality of life and academic performance: New Zealand medical students. J Religion and Health. 2015;54(1):3-19.
Haas GM, Momo AC, Dias TM, Ayodele TA, Schwarzbold ML. Sociodemographic, psychiatric, and personality correlates of non-prescribed use of amphetamine medications for academic performance among medical students. Brazilian J Psychiatry. 2019;41(4):363-4.
Kommelage M, Thabrew H. Student-led peer-assisted learning: The Kuppi experience at the Medical School of the University of Ruhuna in Sri Lanka. Educ Health (Abingdon). 2011;24(2):516.
Isik U, Wouters A, Ter Wee MM, Croiset G, Kusurkar RA. Motivation and academic performance of medical students from ethnic minorities and majority: a comparative study. BMC Med Educ. 2017;17:1-9.
Office for National Statistics. ONS website, statistical bulletin, Religion, England and Wales: Census 2021. Office for National Statistics. 2022.
General Medical Council. The state of medical education and practice in the UK: The Workforce Report. 2022.
Sta. Maria NL, Nizam N, Chowdhury V. Religiosity, gender, and study skills. Coll Student J. 2018;52(3):315-28.
Salem RO, Al-Mously N, Nabil NM, Al-Zalabani AH, Al-Dhawi AF, Al-Hamdan N. Academic and socio-demographic factors influencing students' performance in a new Saudi medical school. Med Teach. 2013;35:S83-S9.
McCabe SE, Knight JR, Teter CJ, Wechsler H. Non-medical use of prescription stimulants among US college students: prevalence and correlates from a national survey. Addiction. 2005;100(1):96-106.
Arria AM, DuPont RL. Nonmedical prescription stimulant use among college students: why we need to do something and what we need to do. J Addict Dis. 2010;29(4):417-26.
Strage AA. Family context variables and the development of self-regulation in college students. Adolescence. 1998;33(129):17-31.
Griffin B, Hu W. Parental career expectations: effect on medical students’ career attitudes over time. Med Educ. 2019;53(6):584-92.
Khoo HE. Implementation of problem-based learning in Asian medical schools and students' perceptions of their experience. Med Educ. 2003;37(5):401-9.
Frambach JM, Driessen EW, Beh P, van der Vleuten CPM. Quiet or questioning? Students' discussion behaviors in student-centered education across cultures. Studies on Higher Educ. 2014;39:1001-21.
Eysenck HJ. The Dynamics of Anxiety and Hysteria. London: Routledge. 1957.
van Houten-Schat MA, Berkhout JJ, van Dijk N, Endedijk MD, Jaarsma ADC, Diemers AD. Self-regulated learning in the clinical context: a systematic review. Med Educ. 2018;52(10):1008-15.
Baarts C, Tulinius C, Reventlow S. Reflexivity—a strategy for a patient-centred approach in general practice. Fam Practice. 2000;17(5):430-4.
Published
How to Cite
License
Copyright (c) 2024 Hamzah Shahid Rafiq, Erik Blair

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- The Author retains copyright in the Work, where the term “Work” shall include all digital objects that may result in subsequent electronic publication or distribution.
- Upon acceptance of the Work, the author shall grant to the Publisher the right of first publication of the Work.
- The Author shall grant to the Publisher and its agents the nonexclusive perpetual right and license to publish, archive, and make accessible the Work in whole or in part in all forms of media now or hereafter known under a Creative Commons Attribution 4.0 International License or its equivalent, which, for the avoidance of doubt, allows others to copy, distribute, and transmit the Work under the following conditions:
- Attribution—other users must attribute the Work in the manner specified by the author as indicated on the journal Web site; with the understanding that the above condition can be waived with permission from the Author and that where the Work or any of its elements is in the public domain under applicable law, that status is in no way affected by the license.
- The Author is able to enter into separate, additional contractual arrangements for the nonexclusive distribution of the journal's published version of the Work (e.g., post it to an institutional repository or publish it in a book), as long as there is provided in the document an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post online a prepublication manuscript (but not the Publisher’s final formatted PDF version of the Work) in institutional repositories or on their Websites prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. Any such posting made before acceptance and publication of the Work shall be updated upon publication to include a reference to the Publisher-assigned DOI (Digital Object Identifier) and a link to the online abstract for the final published Work in the Journal.
- Upon Publisher’s request, the Author agrees to furnish promptly to Publisher, at the Author’s own expense, written evidence of the permissions, licenses, and consents for use of third-party material included within the Work, except as determined by Publisher to be covered by the principles of Fair Use.
- The Author represents and warrants that:
- the Work is the Author’s original work;
- the Author has not transferred, and will not transfer, exclusive rights in the Work to any third party;
- the Work is not pending review or under consideration by another publisher;
- the Work has not previously been published;
- the Work contains no misrepresentation or infringement of the Work or property of other authors or third parties; and
- the Work contains no libel, invasion of privacy, or other unlawful matter.
- The Author agrees to indemnify and hold Publisher harmless from the Author’s breach of the representations and warranties contained in Paragraph 6 above, as well as any claim or proceeding relating to Publisher’s use and publication of any content contained in the Work, including third-party content.
Enforcement of copyright
The IJMS takes the protection of copyright very seriously.
If the IJMS discovers that you have used its copyright materials in contravention of the license above, the IJMS may bring legal proceedings against you seeking reparation and an injunction to stop you using those materials. You could also be ordered to pay legal costs.
If you become aware of any use of the IJMS' copyright materials that contravenes or may contravene the license above, please report this by email to contact@ijms.org
Infringing material
If you become aware of any material on the website that you believe infringes your or any other person's copyright, please report this by email to contact@ijms.org







