Evaluating a Low-Fidelity Anesthesiology Simulation for Airway Management and Cardiac Arrest in Medical Students
DOI:
https://doi.org/10.5195/ijms.2025.2672Keywords:
Medical education, Anesthesiology, Patient simulation, Medical StudentsAbstract
Background: Low-fidelity simulations are cost-effective, accessible tools for medical education. This study describes the development and initial implementation of a low-cost, easy-to-run simulation, assesses participant performance in airway management and ACLS, and reviews qualitative feedback to refine future iterations.
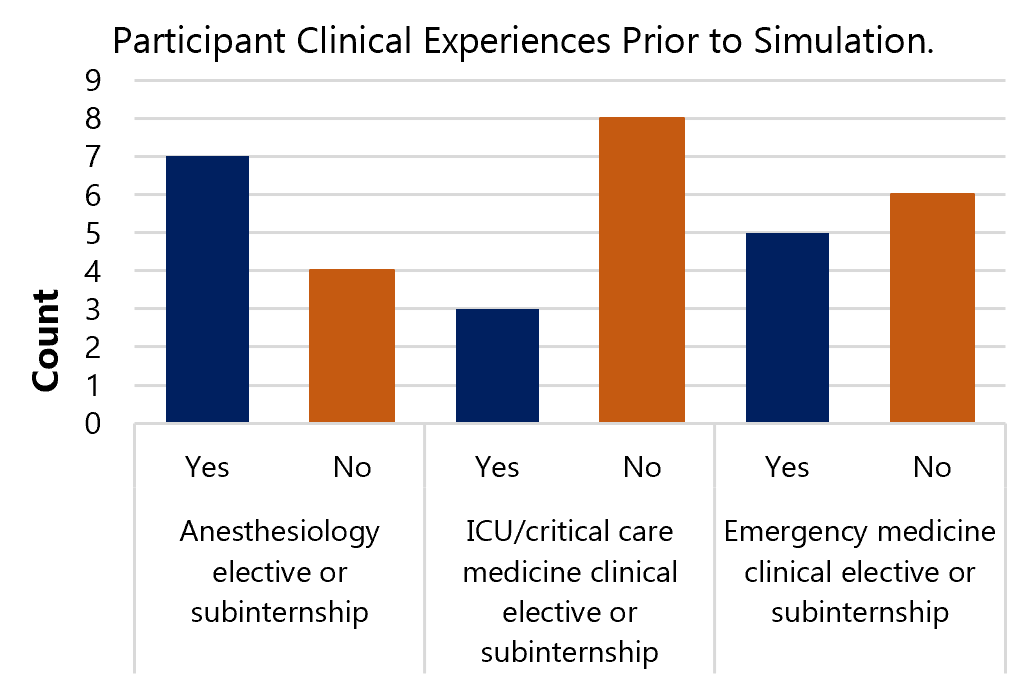
Methods: This single-center, prospective observational study piloted a low-fidelity simulation on difficult airway management and intraoperative cardiac arrest for fourth-year medical students in a three-hour workshop. Participant demographics, simulation performance, and post-simulation feedback were analyzed using proportions and Fisher’s exact test.
Results: A total of eleven medical students participated in the simulation, with most participants scoring in the higher range. No statistically significant findings using the Fisher’s exact test were detected between student performance and past experiences in related fields of anesthesiology, critical care medicine, or emergency medicine. Learners had the most difficulty with adherence to ACLS pathways when managing a simulated cardiac arrest, scoring on average 4.5 ± 1.6 points out of 8. Six of the eleven participants completed the post-simulation survey (55% response rate), primarily giving positive feedback, with all responses indicating agreement that low-fidelity simulations are beneficial learning opportunities for medical students, citing them as helpful to review knowledge.
Conclusion: Low-fidelity simulations provide an underutilized yet effective means for skill development in medical education. ACLS performance gaps may stem from limited practice or situational stress. This simulation requires minimal resources and personnel, making it easily adoptable. Future improvements include a larger sample size, clearer questions, and preparatory materials.
References
Singh H, Kalani M, Acosta-Torres S, El Ahmadieh TY, Loya J, Ganju A. History of simulation in medicine: from Resusci Annie to the Ann Myers Medical Center. Neurosurgery. 2013;73 Suppl 1:9-14.
Dorfling J, Hatton KW, Hassan ZU. Integrating echocardiography into human patient simulator training of anesthesiology residents using a severe pulmonary embolism scenario. Simul Healthc. 2006;1(2):79-83.
Altun D, Ozkan-Seyhan T, Camci E, Sivrikoz N, Orhan-Sungur M. Learning Curves for Two Fiberscopes in Simulated Difficult Airway Scenario with Cumulative Sum Method. Simul Healthc. 2019;14(3):163-168.
Yu CJ, Rigueiro F, Backfish-White K, Cartwright J, Moore C, Mitchell SA, et al. Cricothyrotomy in Acute Upper Gastrointestinal Bleed: A Difficult Airway Simulation Case for Anesthesiology Residents. MedEdPORTAL. 2024;20:11378.
Hong BE, Myo Bui CC, Huang YM, Grogan T, Duval VF, Cannesson M. Implementing COVID-19 Simulation Training for Anesthesiology Residents. MedEdPORTAL. 2022;18:11215.
Asselin M, Lafleur A, Labrecque P, Pellerin H, Tremblay MH, Chiniara G. Simulation of Adult Surgical Cricothyrotomy for Anesthesiology and Emergency Medicine Residents: Adapted for COVID-19. MedEdPORTAL. 2021;17:11134.
Chang CH. Medical simulation is needed in anesthesia training to achieve patient's safety. Korean J Anesthesiol. 2013;64(3):204-211.
Chakravarthy B, Ter Haar E, Bhat SS, McCoy CE, Denmark TK, Lotfipour S. Simulation in medical school education: review for emergency medicine. West J Emerg Med. 2011;12(4):461-466.
Nguyen W, Fromer I, Remskar M, Zupfer E. Development and Implementation of Video-Recorded Simulation Scenarios to Facilitate Case-Based Learning Discussions for Medical Students' Virtual Anesthesiology Clerkship. MedEdPORTAL. 2023;19:11306.
Ellis TA, Bracho DO, Krishnan S. Responding to a Respiratory Complication in the Recovery Room: A Simulation Case for Anesthesiology Students. MedEdPORTAL. 2017;13:10529.
Krishnan S, Kumar N, Diaz E, Thornton I, Ghoddoussi F, Ellis TA 2nd. Anesthesiology Handoff Simulation Case: A Handoff from Intensive Care Unit to Operating Room for Anesthesiology Learners. MedEdPORTAL. 2020;16:10887.
Quick J, Murthy R, Goyal N, Margolis S, Pond G, Jenkins K. Malignant Hyperthermia: An Anesthesiology Simulation Case for Early Anesthesia Providers. MedEdPORTAL. 2017;13:10550.
Ellis TA, Edberg JL, Kumar N, Applefield DJ. Delayed Emergence from Anesthesia: A Simulation Case for Anesthesia Learners. MedEdPORTAL. 2017;13:10628.
Association of American Medical Colleges. Simulation Center Use at Medical Schools. Available from: https://www.aamc.org/data-reports/curriculum-reports/data/simulation-center-use-medical-schools. Last updated 2014; cited April 25, 2024.
Senvisky JM, McKenna RT, Okuda Y. Financing and Funding a Simulation Center. Treasure Island: StatPearls; 2024.
Hippe DS, Umoren RA, McGee A, Bucher SL, Bresnahan BW. A targeted systematic review of cost analyses for implementation of simulation-based education in healthcare. SAGE Open Med. 2020;8:2050312120913451.
Massoth C, Röder H, Ohlenburg H, Hessler M, Zarbock A, Pöpping DM, et al. High-fidelity is not superior to low-fidelity simulation but leads to overconfidence in medical students. BMC Med Educ. 2019;19(1):29.
Philp N, Omran A, Otorkpa MJ, Kirk A. Medical Students' Confidence After "CardioSim": A Low-Fidelity, Peer Role-Play Simulation. Cureus. 2024;16(8):e67192.
Kassutto S, Clancy C, Bennett N, Tsao S. Virtual Simulations to Enhance Medical Student Exposure to Management of Critically Ill Patients. ATS Sch. 2024;5(2):242-246.
Delisle M, Hannenberg AA. Alternatives to High-Fidelity Simulation. Anesthesiol Clin. 2020;38(4):761-773.
The OpenCriticalCare.org Project. Anesthesia & Critical Care Simulation Scenarios for Resource Constrained Settings. Available from: https://opencriticalcare.org/resources/anesthesia-critical-care-simulation-scenarios-for-resource-constrained-settings/. Last updated: September 7, 2022; cited April 25, 2024.
The Accreditation Council for Graduate Medical Education. Anesthesiology Milestones. Available from: https://www.acgme.org/globalassets/pdfs/milestones/anesthesiologymilestones.pdf. Last updated: November 2020; cited April 25, 2024.
Apfelbaum JL, Hagberg CA, Connis RT, Abdelmalak BB, Agarkar M, Dutton RP, et al. 2022 American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway. Anesthesiology. 2022;136(1):31-81.
Panchal AR, Bartos JA, Cabañas JG, Donnino MW, Drennan IR, Hirsch KG, et al. Part 3: Adult Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142(16_suppl_2):S366-S468.
Strom SL, Anderson CL, Yang L, Canales C, Amin A, Lotfipour S, et al. Correlation of Simulation Examination to Written Test Scores for Advanced Cardiac Life Support Testing: Prospective Cohort Study. West J Emerg Med. 2015;16(6):907-912.
Anton NE, Rendina MA, Hennings JM, Stambro R, Stanton-Maxey KJ, Stefanidis D. Association of Medical Students' Stress and Coping Skills with Simulation Performance. Simul Healthc. 2021;16(5):327-333.
Langdorf MI, Strom SL, Yang L, Canales C, Anderson CL, Amin A, et al. High-fidelity simulation enhances ACLS training. Teach Learn Med. 2014;26(3):266-273.
Promes SB, Chudgar SM, Grochowski CO, Shayne P, Isenhour J, Glickman SW, et al. Gaps in procedural experience and competency in medical school graduates. Acad Emerg Med. 2009;16 Suppl 2:S58-S62.
Ko PY, Scott JM, Mihai A, Grant WD. Comparison of a modified longitudinal simulation-based advanced cardiovascular life support to a traditional advanced cardiovascular life support curriculum in third-year medical students. Teach Learn Med. 2011;23(4):324-330.
Nacca N, Holliday J, Ko PY. Randomized trial of a novel ACLS teaching tool: does it improve student performance?. West J Emerg Med. 2014;15(7):913-918.
Ambardekar AP, Rosero EB, Bhoja R, Green J, Rebal BA, Minhajuddin AT, et al. A Randomized Controlled Trial Comparing Learners' Decision-making, Anxiety, and Task Load During a Simulated Airway Crisis Using Two Difficult Airway Aids. Simul Healthc. 2019;14(2):96-103.
Myatra SN, Kalkundre RS, Divatia JV. Optimizing education in difficult airway management: meeting the challenge. Curr Opin Anaesthesiol. 2017;30(6):748-754.
Walsh KL, Yadav A, Cradeur M, Huang H, Lee D, Owusu-Dapaah H, et al. Impact of a Preclinical Medical Student Anesthesiology Elective on the Attitudes and Perceptions of Medical Students Regarding Anesthesiology. Adv Med Educ Pract. 2023;14:1347-1355.
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2025 Kendra Walsh, Christopher Samuel, Shyamal Asher

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- The Author retains copyright in the Work, where the term “Work” shall include all digital objects that may result in subsequent electronic publication or distribution.
- Upon acceptance of the Work, the author shall grant to the Publisher the right of first publication of the Work.
- The Author shall grant to the Publisher and its agents the nonexclusive perpetual right and license to publish, archive, and make accessible the Work in whole or in part in all forms of media now or hereafter known under a Creative Commons Attribution 4.0 International License or its equivalent, which, for the avoidance of doubt, allows others to copy, distribute, and transmit the Work under the following conditions:
- Attribution—other users must attribute the Work in the manner specified by the author as indicated on the journal Web site; with the understanding that the above condition can be waived with permission from the Author and that where the Work or any of its elements is in the public domain under applicable law, that status is in no way affected by the license.
- The Author is able to enter into separate, additional contractual arrangements for the nonexclusive distribution of the journal's published version of the Work (e.g., post it to an institutional repository or publish it in a book), as long as there is provided in the document an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post online a prepublication manuscript (but not the Publisher’s final formatted PDF version of the Work) in institutional repositories or on their Websites prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. Any such posting made before acceptance and publication of the Work shall be updated upon publication to include a reference to the Publisher-assigned DOI (Digital Object Identifier) and a link to the online abstract for the final published Work in the Journal.
- Upon Publisher’s request, the Author agrees to furnish promptly to Publisher, at the Author’s own expense, written evidence of the permissions, licenses, and consents for use of third-party material included within the Work, except as determined by Publisher to be covered by the principles of Fair Use.
- The Author represents and warrants that:
- the Work is the Author’s original work;
- the Author has not transferred, and will not transfer, exclusive rights in the Work to any third party;
- the Work is not pending review or under consideration by another publisher;
- the Work has not previously been published;
- the Work contains no misrepresentation or infringement of the Work or property of other authors or third parties; and
- the Work contains no libel, invasion of privacy, or other unlawful matter.
- The Author agrees to indemnify and hold Publisher harmless from the Author’s breach of the representations and warranties contained in Paragraph 6 above, as well as any claim or proceeding relating to Publisher’s use and publication of any content contained in the Work, including third-party content.
Enforcement of copyright
The IJMS takes the protection of copyright very seriously.
If the IJMS discovers that you have used its copyright materials in contravention of the license above, the IJMS may bring legal proceedings against you seeking reparation and an injunction to stop you using those materials. You could also be ordered to pay legal costs.
If you become aware of any use of the IJMS' copyright materials that contravenes or may contravene the license above, please report this by email to contact@ijms.org
Infringing material
If you become aware of any material on the website that you believe infringes your or any other person's copyright, please report this by email to contact@ijms.org







