Pseudo-Chilblains in Adult Patients with Confirmed COVID-19: A Systematic Review
DOI:
https://doi.org/10.5195/ijms.2023.1648Keywords:
COVID-19, SARS CoV-2, Pernio, Perniosis, Chilblain, Exanthem, Viral, Toes, Pseudo-Chilblains, Severe Acute Respiratory Syndrome Coronavirus 2, equelae, Post-acute sequelae SARS-CoV-2, Sequelae, Complications, Viral pneumonia, 2019-nCoV Infection, SARS-CoV-2 Infection, Coronavirus Disease 2019Abstract
Background: Pseudo-chilblains have been associated with COVID-19. Many reports, however, lack confirmation of COVID-19 infection. While likely associated, all chilblains/chilblain-like lesions during this time should not be assumed to be COVID-19 related. This study examines the characteristics of adults with pseudo-chilblains and confirmed COVID-19.
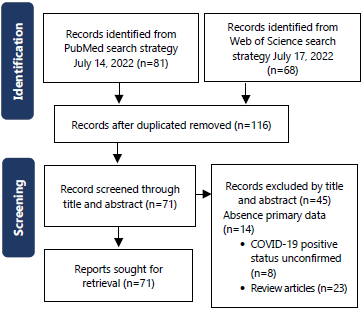
Methods: A systematic review of PubMed/MEDLINE database was performed using the PRISMA guidelines. Adults (>18 years) with confirmed COVID-19 were included. De-identified registries were excluded to avoid duplication. We extracted study design, age, sex, race, geographic location, relationship of COVID-19 diagnosis to chilblains onset, confirmatory testing, hospitalization status, anatomical location, cold/damp exposure, presence/absence/description of pseudo-chilblains symptoms, presence/absence of biopsies/histopathologic findings, tissue IHC/PCR, presence/absence/details of extracutaneous COVID-19 disease, pre-existing chilblains, treatment and resolution timeline. The search was completed in July 2022.
Results: We identified 13 studies (29 patients). In COVID-19-infected adults, pseudo-chilblains were reported primarily from North America and Europe, occurring in both sexes over a wide age-range, affected well and ill patients, favored the hands and feet and could be symptomatic or asymptomatic. Most patients had extracutaneous symptoms. Resolution time ranged from <1 week to >50 days. There was marked variation in treatment strategies and appearance of pseudo-chilblains relative to entire disease course. Biopsies were infrequently performed but findings similar to classical chilblains were described.
Conclusions: Many patients reported as pseudo-chilblains of COVID-19 lack confirmed infection. Infection confirmation, photographic documentation and histopathology are critical to establish homogeneity in reported pseudo-chilblains during this global pandemic. Further work clarifying the relationship of acral eruptions and COVID-19 is necessary.
References
Gupta S, Gupta N, Gupta N. Classification and pathophysiology of cutaneus manifestations of COVID-19. Int J Res Dermatol. 2020;6(4):1-5. DOI: https://doi.org/10.18203/issn.2455-4529.IntJResDermatol20202443
Galván Casas C, Catala A, Carretero Hernández G, Rodríguez‐Jiménez P, Fernández‐Nieto D, Rodríguez‐Villa Lario A, et al. Classification of the cutaneous manifestations of COVID‐19: a rapid prospective nationwide consensus study in Spain with 375 cases. Br J Dermatol. 2020;183(1):71-7. DOI: https://doi.org/10.1111/bjd.19163
AlMahameed A, Pinto DS. Pernio (chilblains). Curr Treat Options Cardiovasc Med. 2008;10(2):128-35. DOI: https://doi.org/10.1007/s11936-008-0014-0
Ghazal S, Litvinov IV, Aljahani N, Jfri A, Netchiporouk E. Cutaneous manifestations of coronavirus disease 2019 (COVID-19) infection-what do we know so far. J Cutan Med Surg. 2020;24(4):416-7. DOI: https://doi.org/10.1177/1203475420928375
Freeman EE, McMahon DE, Lipoff JB, Rosenbach M, Kovarik C, Takeshita J, et al. Pernio-like skin lesions associated with COVID-19: a case series of 318 patients from 8 countries. J Am Acad Dermatol. 2020;83(2):486-92. DOI: https://doi.org/10.1016/j.jaad.2020.05.109
Frumholtz L, Bouaziz JD, Battistella M, et al. Type I interferon response and vascular alteration in chilblain-like lesions during the COVID-19 outbreak. Br J Dermatol. 2021;185(6):1176-85. DOI: https://doi.org/10.1111/bjd.20707
Gómez-Fernández C, López-Sundh AE, González-Vela C, et al. High prevalence of cryofibrinogenemia in patients with chilblains during the COVID-19 outbreak. Int J Dermatol. 2020;59(12):1475-84.
Gao JC, Huang A, Desai A, Safai B, Marmon S. "COVID toes": A true viral phenomenon or a diagnosis without a leg to stand on?. JAAD Int. 2022;9:1-6. DOI: https://doi.org/10.1016/j.jdin.2022.06.012
Le Cleach L, Dousset L, Assier H, Fourati S, Barbarot S, Boulard C, et al. Most chilblains observed during the COVID‐19 outbreak occur in patients who are negative for COVID‐19 on polymerase chain reaction and serology testing. Br J Dermatol. 2020;183(5):866-74. DOI: https://doi.org/10.1111/bjd.19377
Moher, D., Shamseer, L., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., ... & Stewart, L. A. (2015),Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. DOI: https://doi.org/10.1186/2046-4053-4-1
Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, Currie M, Qureshi R, Mattis P, Lisy K, Mu P-F. Chapter 7: Systematic reviews of etiology and risk. In: Aromataris E, Munn Z (Editors). Joanna Briggs Institute Reviewer's Manual. The Joanna Briggs Institute. 2017. Available from https://reviewersmanual.joannabriggs.org/
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. DOI: https://doi.org/10.1136/bmj.n71
Santonja C, Heras F, Núñez L, Requena L. COVID‐19 chilblain‐like lesion: immunohistochemical demonstration of SARS‐CoV‐2 spike protein in blood vessel endothelium and sweat gland epithelium in a PCR‐negative patient. Br J Dermatol. 2020;183(4):778-80. DOI: https://doi.org/10.1111/bjd.19338
Almeida G, Arruda S, Marques E, Michalany N, Sadick N. Presentation and Management of Cutaneous Manifestations of COVID-19. J Drugs Dermatol. 2021:76-83. DOI: https://doi.org/10.36849/JDD.5676
Rubin A, Alamgir M, Rubin J, Rao BK. Chilblain-like lesions with prominent bullae in a patient with COVID-19. BMJ Case Reports CP. 2020;13(11):e237917. DOI: https://doi.org/10.1136/bcr-2020-237917
Recalcati S, Gianotti R, Fantini F. COVID-19: The experience from Italy. Clin Dermatol. 2021;39(1):12-22. DOI: https://doi.org/10.1016/j.clindermatol.2020.12.008
Rekhtman S, Tannenbaum R, Strunk A, Birabaharan M, Wright S, Grbic N, et al. Eruptions and related clinical course among 296 hospitalized adults with confirmed COVID-19. J Am Acad Dermatol. 2021;84(4):946-52. DOI: https://doi.org/10.1016/j.jaad.2020.12.046
Mendez Maestro I, Pena Merino L, Udondo Gonzalez del Tanago B, Aramburu González A, Orbea Sopeña A, Sanchez De Vicente J, et al. Skin manifestations in patients hospitalized with confirmed COVID‐19 disease: a cross‐sectional study in a tertiary hospital. Int J Dermatol. 2020;59(11):1353-7. DOI: https://doi.org/10.1111/ijd.15180
Wee C, Tey HL. Chilblain-like eruption in COVID-19 disease: possible pathogenetic role of temperature. Eur J Dermatol. 2020;1(1). DOI: https://doi.org/10.1684/ejd.2020.3943
Shah I, Stacey SK, Ganne N, Merfeld J. Perniosis in the COVID-19 era. Dermatol Online J. 2021;27(5). DOI: https://doi.org/10.5070/D327553625
Alramthan A, Aldaraji W. Two cases of COVID‐19 presenting with a clinical picture resembling chilblains: first report from the Middle East. Clin Exp Dermatol. 2020;45(6):746-8. DOI: https://doi.org/10.1111/ced.14243
Brancaccio G, Gussetti N, Sasset L, Alaibac M, Tarantello M, Salmaso R, et al. Cutaneous manifestations in a series of 417 patients with SARS-CoV-2 infection: epidemiological and clinical correlates of chilblain like lesions. Pathog Glob Health. 2021;115(7-8):483-6. DOI: https://doi.org/10.1080/20477724.2021.1901040
Gambichler T, Reuther J, Stücker M, Stranzenbach R, Torres‐Reyes C, Schlottmann R, et al. SARS‐CoV‐2 spike protein is present in both endothelial and eccrine cells of a chilblain‐like skin lesion. J Eur Acad Dermatol Venereol. 2021;35(3):e187-9. DOI: https://doi.org/10.1111/jdv.16970
Proietti I, Tolino E, Bernardini N, Mambrin A, Balduzzi V, Marchesiello A, et al. Auricle perniosis as a manifestation of Covid-19 infection. Dermatol Ther. 2020;33(6):e14089. DOI: https://doi.org/10.1111/dth.14089
Ko CJ, Harigopal M, Gehlhausen JR, Bosenberg M, McNiff JM, Damsky W. Discordant anti‐SARS‐CoV‐2 spike protein and RNA staining in cutaneous perniotic lesions suggests endothelial deposition of cleaved spike protein. J Cutan Pathol. 2021;48(1):47-52. DOI: https://doi.org/10.1111/cup.13866
Magro C, Mulvey J, Laurence J, Sanders S, Crowson A, Grossman M, et al. The differing pathophysiologies that underlie COVID‐19‐associated perniosis and thrombotic retiform purpura: a case series. Br J Dermatol. 2021;184(1):141-50. DOI: https://doi.org/10.1111/bjd.19415
Gómez‐Fernández C, López‐Sundh AE, González‐Vela C, Ocejo‐Vinyals JG, Mayor‐Ibarguren A, Salas‐Venero CA, et al. High prevalence of cryofibrinogenemia in patients with chilblains during the COVID‐19 outbreak. Int J Dermatol. 2020;59(12):1475-84. DOI: https://doi.org/10.1111/ijd.15234
McCleskey PE, Zimmerman B, Lieberman A, Liu L, Chen C, Gorouhi F, et al. Epidemiologic analysis of chilblains cohorts before and during the COVID-19 pandemic. JAMA Dermatol. 2021;157(8):947-53. DOI: https://doi.org/10.1001/jamadermatol.2021.2120
Zhang L, Richards A, Barrasa MI, Hughes SH, Young RA, Jaenisch R. Reverse-transcribed SARS-CoV-2 RNA can integrate into the genome of cultured human cells and can be expressed in patient-derived tissues. Proc Natl Acad Sci U S A. 2021;118(21). DOI: https://doi.org/10.1073/pnas.2105968118
Gisondi P, PIaserico S, Bordin C, Alaibac M, Girolomoni G, Naldi L. Cutaneous manifestations of SARS‐CoV‐2 infection: a clinical update. J Eur Acad Dermatol Venereol. 2020;34(11):2499-504. DOI: https://doi.org/10.1111/jdv.16774
Lee DS, Mirmirani P, McCleskey PE, Mehrpouya M, Gorouhi F. Cutaneous manifestations of COVID-19: a systematic review and analysis of individual patient-level data. Dermatol Online J. 2020;26(12). DOI: https://doi.org/10.5070/D32612051347
Kanitakis J, Lesort C, Danset M, Jullien D. Chilblain-like acral lesions during the COVID-19 pandemic (“COVID toes”): Histologic, immunofluorescence, and immunohistochemical study of 17 cases. J Am Acad Dermatol. 2020;83(3):870-5. DOI: https://doi.org/10.1016/j.jaad.2020.05.145
Goette DK. Chilblains (perniosis). J Am Acad Dermatol. 1990;23(2):257-62. DOI: https://doi.org/10.1016/0190-9622(90)70209-Z
Ko CJ, Harigopal M, Damsky W, Gehlhausen JR, Bosenberg M, Patrignelli R, et al. Perniosis during the COVID‐19 pandemic: Negative anti‐SARS‐CoV‐2 immunohistochemistry in six patients and comparison to perniosis before the emergence of SARS‐CoV‐2. J Cutan Pathol. 2020;47(11):997-1002. DOI: https://doi.org/10.1111/cup.13830
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2023 Seon Hayles, Kelsey Williams, Nidhi Thomas, Jabari Morgan, Donna Braham, Maxine Gossell Williams, Jonathan D. Ho

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- The Author retains copyright in the Work, where the term “Work” shall include all digital objects that may result in subsequent electronic publication or distribution.
- Upon acceptance of the Work, the author shall grant to the Publisher the right of first publication of the Work.
- The Author shall grant to the Publisher and its agents the nonexclusive perpetual right and license to publish, archive, and make accessible the Work in whole or in part in all forms of media now or hereafter known under a Creative Commons Attribution 4.0 International License or its equivalent, which, for the avoidance of doubt, allows others to copy, distribute, and transmit the Work under the following conditions:
- Attribution—other users must attribute the Work in the manner specified by the author as indicated on the journal Web site; with the understanding that the above condition can be waived with permission from the Author and that where the Work or any of its elements is in the public domain under applicable law, that status is in no way affected by the license.
- The Author is able to enter into separate, additional contractual arrangements for the nonexclusive distribution of the journal's published version of the Work (e.g., post it to an institutional repository or publish it in a book), as long as there is provided in the document an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post online a prepublication manuscript (but not the Publisher’s final formatted PDF version of the Work) in institutional repositories or on their Websites prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. Any such posting made before acceptance and publication of the Work shall be updated upon publication to include a reference to the Publisher-assigned DOI (Digital Object Identifier) and a link to the online abstract for the final published Work in the Journal.
- Upon Publisher’s request, the Author agrees to furnish promptly to Publisher, at the Author’s own expense, written evidence of the permissions, licenses, and consents for use of third-party material included within the Work, except as determined by Publisher to be covered by the principles of Fair Use.
- The Author represents and warrants that:
- the Work is the Author’s original work;
- the Author has not transferred, and will not transfer, exclusive rights in the Work to any third party;
- the Work is not pending review or under consideration by another publisher;
- the Work has not previously been published;
- the Work contains no misrepresentation or infringement of the Work or property of other authors or third parties; and
- the Work contains no libel, invasion of privacy, or other unlawful matter.
- The Author agrees to indemnify and hold Publisher harmless from the Author’s breach of the representations and warranties contained in Paragraph 6 above, as well as any claim or proceeding relating to Publisher’s use and publication of any content contained in the Work, including third-party content.
Enforcement of copyright
The IJMS takes the protection of copyright very seriously.
If the IJMS discovers that you have used its copyright materials in contravention of the license above, the IJMS may bring legal proceedings against you seeking reparation and an injunction to stop you using those materials. You could also be ordered to pay legal costs.
If you become aware of any use of the IJMS' copyright materials that contravenes or may contravene the license above, please report this by email to contact@ijms.org
Infringing material
If you become aware of any material on the website that you believe infringes your or any other person's copyright, please report this by email to contact@ijms.org







