A Narrative Review of Women in Medicine Interest Groups at the Pre-Medical, Graduate, and Post-Graduate Medical Education Levels
DOI:
https://doi.org/10.5195/ijms.2025.2281Keywords:
Toolkit, Women, Medicine, Education, Medical, Undergraduate, Pre-Medical, Graduate, Medical Education, Interest GroupsAbstract
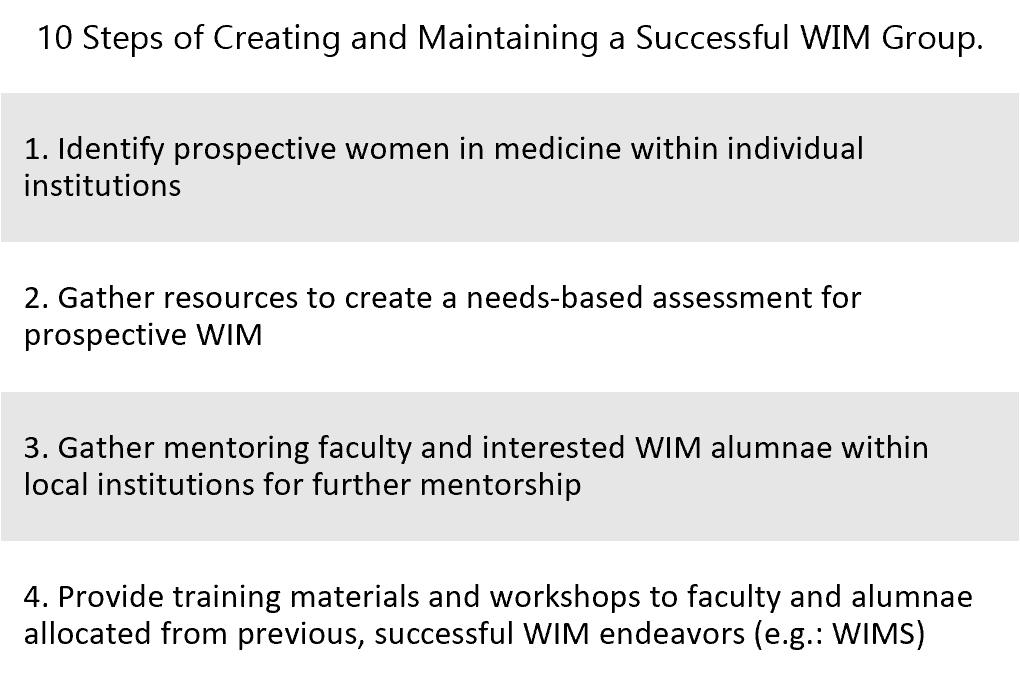
Women in Medicine (WIM) interest groups can provide collaboration and support for the professional development of women as they navigate the gender inequities that persist in the healthcare workplace. This narrative review assesses successful methods used by multiple institutions to form groups and toolkits catered to women's empowerment. Medical career education was stratified into three levels: Pre-Medical, Graduate, and Post-graduate Medical Education. Keyword literature search on peer-reviewed platforms including Google Scholar, PubMed, OVID, Ebsco, and gray literature (i.e. medical societies toolkits) was used to identify applicable articles. We aimed to develop a toolkit derived from literature findings consisting of a list of ten steps for creating and maintaining a successful WIM group based on successful measures reported in the literature. Mentorship, adequate resources, administrative supportive efforts, networking, and safe spaces were found to be essential to career growth for women on each of the pre-established educational levels.
References
1. Bauman Bauman MD, Howell LP, Villablanca AC. The Women in Medicine and Health Science program: an innovative initiative to support female faculty at the University of California Davis School of Medicine. Acad Med. 2014;89(11):1462–1466.
2. Boyle P. Nation's Physician Workforce Evolves: More Women, a Bit Older, and toward Different Specialties. AAMC. 2021 Feb 2. Available from: https://www.aamc.org/news-insights/nation-s-physician-workforce-evolves-more-women-bit-older-and-toward-different-specialties
3. Mangurian C, Linos E, Sarkar U, Rodriguez C, Jagsi R. What's Holding Women in Medicine Back from Leadership. Harvard Business Review. 2018 Nov 7. Available from: https://hbr.org/2018/06/whats-holding-women-in-medicine-back-from-leadership
4. Lautenberger D, Raezer C, Bunton S. The underrepresentation of women in leadership positions at U.S. medical schools. AAMC Analysis in Brief. 2015;15(2). Available from: https://www.aamc.org/data/aib/425010/february2015.html
5. Jagsi R, Guancial EA, Worobey CC, Henault LE, Chang Y, Starr R, et al. The gender gap in authorship of academic medical literature—A 35-year perspective. N Engl J Med. 2006;355(3):281–287.
6. Butkus R, Serchen J, Moyer DV, Bornstein SS, Hingle ST, Health and Public Policy Committee of the American College of Physicians, et al. Achieving gender equity in physician compensation and career advancement: A position paper of the American College of Physicians. Ann Intern Med. 2018;168(10):721–723.
7. Berg S. Challenges Faced by Women Physicians Don't Disappear with Age. American Medical Association. 2020 Jun 16. Available from: https://www.ama-assn.org/delivering-care/health-equity/challenges-faced-women-physicians-don-t-disappear-age
8. Shillcutt SK, Parangi S, Diekman S, et al. Survey of women physicians’ experience with elected leadership positions. Health Equity. 2019;3:162–168.
9. Kilminster S, Downes J, Gough B, Murdoch-Eaton D, Roberts T. Women in medicine—is there a problem? A literature review of the changing gender composition, structures and occupational cultures in medicine. Med Educ. 2007;41(1):39–49.
10. Gasparyan AY, Ayvazyan L, Blackmore H, Kitas GD. Writing a narrative biomedical review: considerations for authors, peer reviewers, and editors. Rheumatol Int. 2011;31(11):1409–1417.
11. Penny M, Jeffries R, Grant J, Davies SC. Women and academic medicine: a review of the evidence on female representation. J R Soc Med. 2014;107(7):259–263.
12. Gautam M. Women in medicine: stresses and solutions. West J Med. 2001;174(1):37–41.
13. Grace MK. Parting ways: Sex-based differences in premedical attrition. Soc Sci Med. 2019;230:222–233.
14. Rosenthal L, Levy SR, London B, Lobel M, Bazile C. In pursuit of the MD: The impact of role models, identity compatibility, and belonging among undergraduate women. Sex Roles. 2013;68(7–8):464–473.
15. Berge J, Macheledt K, Watson S, Dorr H, et al. Using a community-based participatory approach to address gender equity in academic medicine: The Center for Women in Medicine and Science at the University of Minnesota. Acad Med. 2021. Advance online publication.
16. Helitzer DL, Newbill SL, Cardinali G, Morahan PS, Chang S, Magrane D. Narratives of participants in national career development programs for women in academic medicine: identifying the opportunities for strategic investment. J Womens Health. 2016;25(4):360–370.
17. Choo EK, Kass D, Westergaard M, Watts SH, Berwald N, Regan L, et al. Best practice recommendations to support the hiring, recruitment, and advancement of women physicians in emergency medicine. Acad Emerg Med. 2016;23(11):1203–1209.
18. Santhosh L, Harleman E, Venado A, Farrand E, Gilbreth ME, Keenan BP, et al. Strategies for forming effective women's groups. Clin Teach. 2021;18(2):126–130.
19. Ibrahim H, Stadler DJ, Archuleta S, Anglade P, Cofrancesco J Jr. Twelve tips for developing and running a successful women's group in international academic medicine. Med Teach. 2019;41(11):1239–1244.
20. Hinson HE, Gonzales NR. On increasing the visibility of women and other groups underrepresented in medicine: To be it, you must see it. Neurology. 2020;95(22):991–992.
21. Singhal D, Bank AM, Poorman JA, Doshi TL, Parekh R, Parangi S, et al. Representation of women plenary speakers at the American Academy of Neurology Annual Meeting. Neurology. 2020;95(22):e3045–e3059.
22. Zhong L, Lee K, Baggstrom MQ, Bhayani RK. Investing in women trainees: Building a Women in Medicine Group at an academic institution. J Med Internet Res. 2023;25:e47783.
23. Pérez-Sánchez S, Madueño SE, Montaner J. Gender gap in the leadership of health institutions: The influence of hospital-level factors. Health Equity. 2021;5(1):521–525.
Published
How to Cite
License
Copyright (c) 2025 Sarah Bhagudas, Alisha Crump, Gabriela Azevedo Sansoni, DeeDee Rubert, Marah Kays, Shikha Jain, Rakhee Bhayani

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- The Author retains copyright in the Work, where the term “Work” shall include all digital objects that may result in subsequent electronic publication or distribution.
- Upon acceptance of the Work, the author shall grant to the Publisher the right of first publication of the Work.
- The Author shall grant to the Publisher and its agents the nonexclusive perpetual right and license to publish, archive, and make accessible the Work in whole or in part in all forms of media now or hereafter known under a Creative Commons Attribution 4.0 International License or its equivalent, which, for the avoidance of doubt, allows others to copy, distribute, and transmit the Work under the following conditions:
- Attribution—other users must attribute the Work in the manner specified by the author as indicated on the journal Web site; with the understanding that the above condition can be waived with permission from the Author and that where the Work or any of its elements is in the public domain under applicable law, that status is in no way affected by the license.
- The Author is able to enter into separate, additional contractual arrangements for the nonexclusive distribution of the journal's published version of the Work (e.g., post it to an institutional repository or publish it in a book), as long as there is provided in the document an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post online a prepublication manuscript (but not the Publisher’s final formatted PDF version of the Work) in institutional repositories or on their Websites prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. Any such posting made before acceptance and publication of the Work shall be updated upon publication to include a reference to the Publisher-assigned DOI (Digital Object Identifier) and a link to the online abstract for the final published Work in the Journal.
- Upon Publisher’s request, the Author agrees to furnish promptly to Publisher, at the Author’s own expense, written evidence of the permissions, licenses, and consents for use of third-party material included within the Work, except as determined by Publisher to be covered by the principles of Fair Use.
- The Author represents and warrants that:
- the Work is the Author’s original work;
- the Author has not transferred, and will not transfer, exclusive rights in the Work to any third party;
- the Work is not pending review or under consideration by another publisher;
- the Work has not previously been published;
- the Work contains no misrepresentation or infringement of the Work or property of other authors or third parties; and
- the Work contains no libel, invasion of privacy, or other unlawful matter.
- The Author agrees to indemnify and hold Publisher harmless from the Author’s breach of the representations and warranties contained in Paragraph 6 above, as well as any claim or proceeding relating to Publisher’s use and publication of any content contained in the Work, including third-party content.
Enforcement of copyright
The IJMS takes the protection of copyright very seriously.
If the IJMS discovers that you have used its copyright materials in contravention of the license above, the IJMS may bring legal proceedings against you seeking reparation and an injunction to stop you using those materials. You could also be ordered to pay legal costs.
If you become aware of any use of the IJMS' copyright materials that contravenes or may contravene the license above, please report this by email to contact@ijms.org
Infringing material
If you become aware of any material on the website that you believe infringes your or any other person's copyright, please report this by email to contact@ijms.org







