Burnout in Ophthalmology Residents in a Tertiary Referral Hospital in Mexico City
DOI:
https://doi.org/10.5195/ijms.2025.2794Keywords:
burnout, Ophthalmology, residents, Mental Health, Emotional exhaustion , Depersonalization, Work-related stress, Sleep deprivation, Medical errors, MexicoAbstract
Background: Burnout is a syndrome conceptualized as a consequence of chronic workplace stress and is characterized by three dimensions: emotional exhaustion, depersonalization, and reduced personal accomplishment. The Maslach Burnout Inventory (MBI) is the most widely used instrument to assess burnout. Due to cultural, political, and sociocultural factors, burnout rates are reported to be higher in Mexico. This study aimed to determine the prevalence of burnout and the factors associated with its development among residents in general ophthalmology and subspecialties at the Asociación Para Evitar la Ceguera (APEC) in Mexico using the MBI.
Methods: A cross-sectional survey was conducted using Google Forms and distributed via social networks and email between January and March 2023 to residents training at APEC. The survey consisted of five sections, including the MBI. Data analysis was performed using the SPSS statistical package.
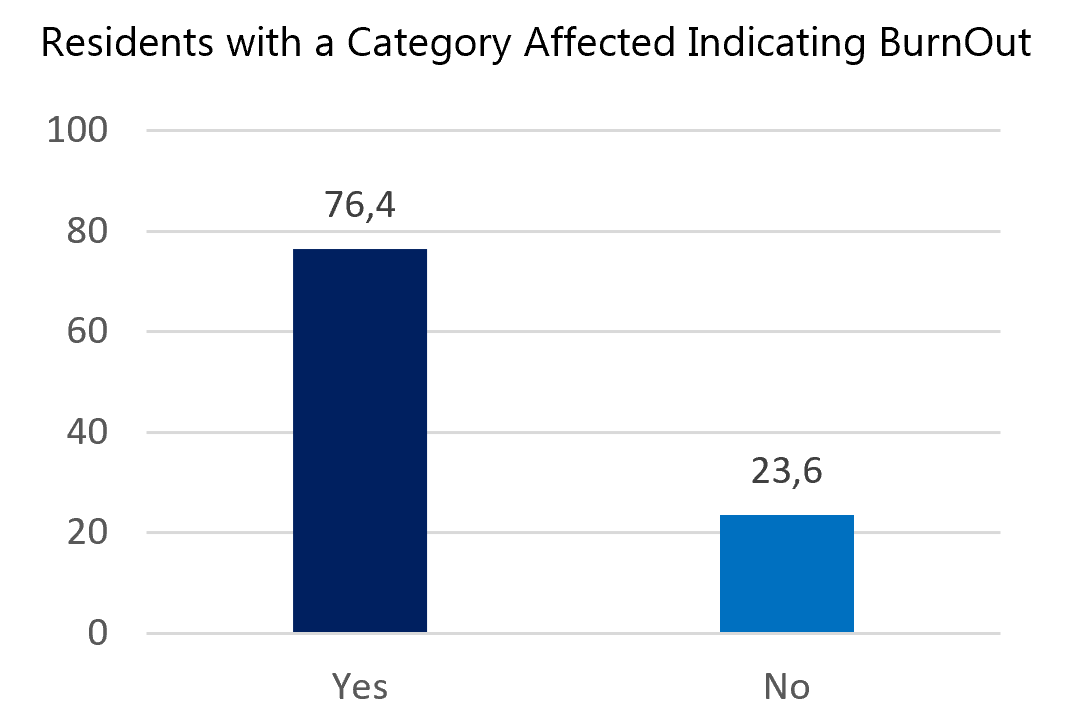
Results: A total of 55 responses were obtained from 122 residents, yielding a response rate of 45%. The prevalence of burnout was 76% (95% CI: 0.65–0.88). Factors significantly associated with burnout included lack of sleep, self-perception of an unhealthy diet, and the number of days per week spent providing consultations. Additionally, burnout was associated with residents’ self-perception of having made medical errors.
Conclusion: Burnout is highly prevalent among ophthalmology residents. Several factors may contribute to its development, particularly sleep deprivation and increased workload. Conducting studies of this nature is essential to identify risk factors and to design effective interventions aimed at improving the well-being and performance of this population.
References
1. Rodrigues H, Cobucci R, Oliveira A, et al. Burnout syndrome among medical residents: a systematic review and meta-analysis. PLoS One. 2018;13(11):e0206840.
2. Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251(6):995–1000.
3. World Health Organization. Burn-out an occupational phenomenon: International Classification of Diseases. 2019 May. Available from: World Health Organization website. Cited Nov 2, 2023.
4. Feng S, Taravati P, Ding L, Menda S. Burnout in ophthalmology residency: a national survey. J Acad Ophthalmol. 2018;10(1):e98–e107.
5. Alotaibi AK, Alsalim A, Alruwaili F, et al. Burnout during ophthalmology residency training: a national survey in Saudi Arabia. Saudi J Ophthalmol. 2019;33(2):130–4.
6. Aguilar-Nájera O, Zamora-Nava LE, Grajales-Figueroa G, Valdovinos-Díaz MÁ, Téllez-Ávila FI. Prevalence of burnout syndrome in gastroenterologists and endoscopists: results of a national survey in Mexico. Postgrad Med. 2020;132(3):275–81.
7. Gil-Monte PR. Validez factorial de la adaptación al español del Maslach Burnout Inventory-General Survey. Salud Publica Mex. 2002;44(1):33–40.
8. Terrone J, et al. Síndrome de burnout en médicos residentes del Hospital General de Durango, México. Rev Med Inst Mex Seguro Soc. 2016;54(2):242–8.
9. Cerpa B, et al. Correlación entre factores sociofamiliares y el síndrome de burnout en residentes y médicos de una unidad de medicina familiar. Arch Med Fam. 2020;24(1):31–6.
10. Saborío L, Hidalgo L. Síndrome de burnout. Med Leg Costa Rica. 2015;32(1):119–24.
11. Centers for Disease Control and Prevention. Are you getting enough sleep? 2022. Available from: CDC website. Cited Nov 2, 2023.
12. Watson NF, et al. Recommended amount of sleep for a healthy adult: a joint consensus statement. Sleep. 2015;38(6):843–4.
13. Stewart NH, Arora VM. The impact of sleep and circadian disorders on physician burnout. Chest. 2019;156(5):1022–30.
14. Trockel MT, Menon NK, Rowe SG, et al. Assessment of physician sleep and wellness, burnout, and clinically significant medical errors. JAMA Netw Open. 2020;3(12):e2028111.
15. Kancherla BS, et al. Sleep, fatigue and burnout among physicians: an American Academy of Sleep Medicine position statement. J Clin Sleep Med. 2020;16(5):803–5.
16. National Health Service. Eating a balanced diet. 2022. Available from: NHS website. Cited Nov 2, 2023.
17. Esquivel MK. Nutrition strategies for reducing risk of burnout among physicians and health care professionals. Am J Lifestyle Med. 2021;15(2):126–9.
18. Melamed S, Shirom A, Toker S, Berliner S, Shapira I. Burnout and risk of cardiovascular disease. Psychol Bull. 2006;132(3):327–53.
19. Scheepers R, Silkens M, van den Berg J, Lombarts K. Associations between job demands, job resources and patient-related burnout among physicians. BMJ Open. 2020;10(9):e038466.
20. Busireddy KR, et al. Efficacy of interventions to reduce resident physician burnout: a systematic review. J Grad Med Educ. 2017;9(3):294–301.
21. Menon NK, Shanafelt TD, Sinsky CA, et al. Association of physician burnout with suicidal ideation and medical errors. JAMA Netw Open. 2020;3(12):e2028780.
22. Al-Ghunaim TA, Johnson J, Biyani CS, Alshahrani KM, Dunning A, O’Connor DB. Surgeon burnout, impact on patient safety and professionalism. Am J Surg. 2022;224(1 Pt A):228–38.
23. Gualano MR, Sinigaglia T, Lo Moro G, et al. The burden of burnout among healthcare professionals during the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18:8172.
24. Jalili M, Niroomand M, Hadavand F, Zeinali K, Fotouhi A. Burnout among healthcare professionals during COVID-19 pandemic. Int Arch Occup Environ Health. 2021;94(6):1345–52.
25. Shopen N, Schneider A, Mordechai RA, et al. Emergency medicine physician burnout before and during the COVID-19 pandemic. Isr J Health Policy Res. 2022;11(1):30.
26. Aryankhesal A, Mohammadibakhsh R, Hamidi Y, et al. Interventions on reducing burnout in physicians and nurses. Med J Islam Repub Iran. 2019;33:77.
27. Galaiya R, Kinross J, Arulampalam T. Factors associated with burnout syndrome in surgeons. Ann R Coll Surg Engl. 2020;102(6):401–7.
28. Chan MK, Chew QH, Sim K. Burnout and associated factors in psychiatry residents. Int J Med Educ. 2019;10:149–60.
29. Yates SW. Physician stress and burnout. Am J Med. 2019;133(2):160–4.
30. Low ZX, Yeo KA, Sharma VK, et al. Prevalence of burnout in medical and surgical residents. Int J Environ Res Public Health. 2019;16(9):1479.
31. Shah HP, Salehi PP, Ihnat J, et al. Resident burnout and well-being in otolaryngology and other surgical specialties. Otolaryngol Head Neck Surg. 2023;168(2):165–79.
Downloads
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2025 Lourdes Adriana Medina-Gaona, Gerardo García Aguirre, Guillermo Salcedo Villanueva, Flor Angélica Jacome - Gutierrez

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- The Author retains copyright in the Work, where the term “Work” shall include all digital objects that may result in subsequent electronic publication or distribution.
- Upon acceptance of the Work, the author shall grant to the Publisher the right of first publication of the Work.
- The Author shall grant to the Publisher and its agents the nonexclusive perpetual right and license to publish, archive, and make accessible the Work in whole or in part in all forms of media now or hereafter known under a Creative Commons Attribution 4.0 International License or its equivalent, which, for the avoidance of doubt, allows others to copy, distribute, and transmit the Work under the following conditions:
- Attribution—other users must attribute the Work in the manner specified by the author as indicated on the journal Web site; with the understanding that the above condition can be waived with permission from the Author and that where the Work or any of its elements is in the public domain under applicable law, that status is in no way affected by the license.
- The Author is able to enter into separate, additional contractual arrangements for the nonexclusive distribution of the journal's published version of the Work (e.g., post it to an institutional repository or publish it in a book), as long as there is provided in the document an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post online a prepublication manuscript (but not the Publisher’s final formatted PDF version of the Work) in institutional repositories or on their Websites prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. Any such posting made before acceptance and publication of the Work shall be updated upon publication to include a reference to the Publisher-assigned DOI (Digital Object Identifier) and a link to the online abstract for the final published Work in the Journal.
- Upon Publisher’s request, the Author agrees to furnish promptly to Publisher, at the Author’s own expense, written evidence of the permissions, licenses, and consents for use of third-party material included within the Work, except as determined by Publisher to be covered by the principles of Fair Use.
- The Author represents and warrants that:
- the Work is the Author’s original work;
- the Author has not transferred, and will not transfer, exclusive rights in the Work to any third party;
- the Work is not pending review or under consideration by another publisher;
- the Work has not previously been published;
- the Work contains no misrepresentation or infringement of the Work or property of other authors or third parties; and
- the Work contains no libel, invasion of privacy, or other unlawful matter.
- The Author agrees to indemnify and hold Publisher harmless from the Author’s breach of the representations and warranties contained in Paragraph 6 above, as well as any claim or proceeding relating to Publisher’s use and publication of any content contained in the Work, including third-party content.
Enforcement of copyright
The IJMS takes the protection of copyright very seriously.
If the IJMS discovers that you have used its copyright materials in contravention of the license above, the IJMS may bring legal proceedings against you seeking reparation and an injunction to stop you using those materials. You could also be ordered to pay legal costs.
If you become aware of any use of the IJMS' copyright materials that contravenes or may contravene the license above, please report this by email to contact@ijms.org
Infringing material
If you become aware of any material on the website that you believe infringes your or any other person's copyright, please report this by email to contact@ijms.org







