Insomnia Prevalence and Risk Factors Among Hispanic University Staff in Ecuador: A Cross-Sectional Study
DOI:
https://doi.org/10.5195/ijms.2025.2814Keywords:
Insomnia, Risk factors, university, Sleep Disorders, prevalenceAbstract
Background: Insomnia, characterized by difficulty initiating or maintaining sleep, is a common condition that adversely affects health, productivity, and overall well-being. This study aimed to determine the prevalence and associated risk factors of insomnia among Hispanic university staff at a higher education institution in Ecuador.
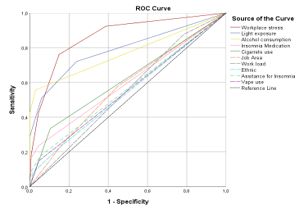
Methods: A cross-sectional study was conducted between August 2023 and February 2024, including 385 university employees. Participants completed an anonymous survey collecting demographic, lifestyle, occupational, and sleep-related data. Sleep quality and insomnia severity were assessed using the Pittsburgh Sleep Quality Index (PSQI) and the Insomnia Severity Index (ISI). Data were analyzed using descriptive statistics, Spearman correlations, logistic regression, and Receiver Operating Characteristic (ROC) curve analysis to identify predictors of clinically significant insomnia (ISI > 14).
Results: The prevalence of insomnia was 65.2%, with mean PSQI and ISI scores of 8.8 ± 5 and 11.5 ± 7, respectively. Severe insomnia affected 2.9% of participants. Higher insomnia scores were significantly correlated with workplace stress, workload, ethnicity, light exposure during sleep, and use of insomnia medication. Logistic regression identified workplace stress and light exposure as the strongest predictors of insomnia. ROC analysis indicated workplace stress had the greatest discriminative ability (AUC = 0.864), followed by light exposure (AUC = 0.789).
Conclusion: A high prevalence of clinically significant insomnia was observed among university staff, primarily linked to workplace stress and nighttime light exposure. Targeted interventions addressing these factors could improve sleep health and overall well-being. Further studies in diverse populations are needed to validate these findings.
References
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). 5th ed. Arlington, TX: American Psychiatric Association Publishing; 2013.
2. Vargas PA, Flores M, Robles E. Sleep quality and body mass index in college students: the role of sleep disturbances. J Am Coll Health. 2014;62(8):534–41.
3. Ford DE. Epidemiologic study of sleep disturbances and psychiatric disorders. JAMA. 1989;262(11):1479.
4. Han X, Zhou E, Liu D. Electronic media use and sleep quality: updated systematic review and meta-analysis. J Med Internet Res. 2024;26:e48356.
5. Lund L, Sølvhøj IN, Danielsen D, Andersen S. Electronic media use and sleep in children and adolescents in Western countries: a systematic review. BMC Public Health. 2021;21:1598.
6. Riehm KE, Rojo-Wissar DM, Feder KA, et al. E-cigarette use and sleep-related complaints among youth. J Adolesc. 2019;76:48–54.
7. Wang S, Nandy RR, Rossheim ME. Associations between e-cigarette use and sleep health among adults in the United States, NHANES 2015–2018. Sleep Med. 2024;114:220–8.
8. Walker M. Why We Sleep: Unlocking the Power of Sleep and Dreams. New York: Scribner; 2017.
9. Rana A, Soodan V. Effect of occupational and personal stress on job satisfaction, burnout, and health: a cross-sectional analysis of college teachers in Punjab, India. Indian J Occup Environ Med. 2019;23(3):133.
10. Grandner MA, Hale L, Jackson N, Patel NP, Gooneratne NS, Troxel WM. Perceived racial discrimination as an independent predictor of sleep disturbance and daytime fatigue. Behav Sleep Med. 2012;10(4):235–49.
11. Sateia MJ. International classification of sleep disorders-third edition: highlights and modifications. Chest. 2014;146(5):1387–94.
12. Sivertsen B, Hysing M, Harvey AG, Petrie KJ. The epidemiology of insomnia and sleep duration across mental and physical health: the SHoT study. Front Psychol. 2021;12:662572.
13. Yip T, Cheon YM. Sleep, psychopathology and cultural diversity. Curr Opin Psychol. 2020;34:123–7.
14. Jackson CL, Powell-Wiley TM, Gaston SA, Andrews MR, Tamura K, Ramos A. Racial/ethnic disparities in sleep health and potential interventions among women in the United States. J Womens Health (Larchmt). 2020;29(3):435–42.
15. Pereira C, Almeida C, Veiga N, Amaral O. Prevalence and determinants of insomnia symptoms among schoolteachers. Aten Primaria. 2014;46:118–22.
16. Yardi N, Adsule S. A cross-sectional observational study to determine the prevalence of insomnia amongst Indian corporate employees. J Assoc Physicians India. 2015;63(10):20–5.
17. Guan YQ, Zhang M, Zhang X, Zhao ZP, Huang ZJ, Li C, et al. Association between alcohol consumption and insomnia in employed floating population in China. Zhonghua Yu Fang Yi Xue Za Zhi. 2021;55(9):1114–22.
18. Zheng D, Yuan X, Ma C, Liu Y, VanEvery H, Sun Y, et al. Alcohol consumption and sleep quality: a community-based study. Public Health Nutr. 2021;24(15):4851–8.
19. Hipson WE, Fisher DJ. The association between acute stress-related insomnia and alcohol use. Sleep Health. 2016;2(3):246–52.
20. Li XM, Cui SY, Song Y, Wu JH, Wang YB, Wang LH, Yuan JX. Association between occupational stress and insomnia among steel workers. J Environ Occup Med. 2019;36(8):710–7.
21. Kim H, Kim B, Min K, Min J, Hwang S, Park S. Association between job stress and insomnia in Korean workers. J Occup Health. 2011;53(3):164–74.
22. Cabral LGL, Queiroz TN, Pol-Fachin L, Santos ARL. Digital technology and its impacts on sleep quality and academic performance during the pandemic. Arq Neuropsiquiatr. 2022;80(10):1052–6.
Downloads
Published
Versions
- 2025-12-19 (2)
- 2025-10-20 (1)
How to Cite
License
Copyright (c) 2025 Carlos Rodriguez, Danny Japon, Linker Viñan, Presley Gruezo, Michelle Hidalgo, Ricardo Moran, Rocio Santibañez

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- The Author retains copyright in the Work, where the term “Work” shall include all digital objects that may result in subsequent electronic publication or distribution.
- Upon acceptance of the Work, the author shall grant to the Publisher the right of first publication of the Work.
- The Author shall grant to the Publisher and its agents the nonexclusive perpetual right and license to publish, archive, and make accessible the Work in whole or in part in all forms of media now or hereafter known under a Creative Commons Attribution 4.0 International License or its equivalent, which, for the avoidance of doubt, allows others to copy, distribute, and transmit the Work under the following conditions:
- Attribution—other users must attribute the Work in the manner specified by the author as indicated on the journal Web site; with the understanding that the above condition can be waived with permission from the Author and that where the Work or any of its elements is in the public domain under applicable law, that status is in no way affected by the license.
- The Author is able to enter into separate, additional contractual arrangements for the nonexclusive distribution of the journal's published version of the Work (e.g., post it to an institutional repository or publish it in a book), as long as there is provided in the document an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post online a prepublication manuscript (but not the Publisher’s final formatted PDF version of the Work) in institutional repositories or on their Websites prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. Any such posting made before acceptance and publication of the Work shall be updated upon publication to include a reference to the Publisher-assigned DOI (Digital Object Identifier) and a link to the online abstract for the final published Work in the Journal.
- Upon Publisher’s request, the Author agrees to furnish promptly to Publisher, at the Author’s own expense, written evidence of the permissions, licenses, and consents for use of third-party material included within the Work, except as determined by Publisher to be covered by the principles of Fair Use.
- The Author represents and warrants that:
- the Work is the Author’s original work;
- the Author has not transferred, and will not transfer, exclusive rights in the Work to any third party;
- the Work is not pending review or under consideration by another publisher;
- the Work has not previously been published;
- the Work contains no misrepresentation or infringement of the Work or property of other authors or third parties; and
- the Work contains no libel, invasion of privacy, or other unlawful matter.
- The Author agrees to indemnify and hold Publisher harmless from the Author’s breach of the representations and warranties contained in Paragraph 6 above, as well as any claim or proceeding relating to Publisher’s use and publication of any content contained in the Work, including third-party content.
Enforcement of copyright
The IJMS takes the protection of copyright very seriously.
If the IJMS discovers that you have used its copyright materials in contravention of the license above, the IJMS may bring legal proceedings against you seeking reparation and an injunction to stop you using those materials. You could also be ordered to pay legal costs.
If you become aware of any use of the IJMS' copyright materials that contravenes or may contravene the license above, please report this by email to contact@ijms.org
Infringing material
If you become aware of any material on the website that you believe infringes your or any other person's copyright, please report this by email to contact@ijms.org







