Clinical Audits in Medical Education: Barriers and Opportunities Among Jordanian Medical Students
DOI:
https://doi.org/10.5195/ijms.2025.3042Keywords:
Clinical Audit, Education Medical, Medical Student, Quality improvement, Evidence-Based PracticeAbstract
Background: Clinical audits are crucial for enhancing healthcare quality, but various obstacles can restrict their implementation. This study aims to examine barriers to the implementation of clinical audits among medical students and interns.
Methods: We conducted a cross-sectional online survey involving 727 clinical-year medical students (4th–6th year) and interns in Jordan from six Jordanian universities between August and November 2023. Participants completed a self-administered online questionnaire covering demographics, knowledge of clinical audits, perspectives on clinical audits, and barriers to conducting them.
Results: Of the 727 participants (58.2% male; 35.5% in their 6th year), only 7.3% had engaged in clinical audits, despite 69.5% identifying personal development and 64.8% recognizing healthcare improvement as motivations. Key barriers included time constraints (78%), academic pressure (79%), and a lack of institutional support (80%), while 59.2% felt their curriculum left them underprepared. Awareness of audit objectives was limited, with 48.4% disagreeing that they understood audit objectives. Fear of criticism was commonly reported, with 70.7% agreeing or strongly agreeing that this discouraged their participation. Multivariable logistic regression adjusted for university, academic year, GPA, and gender showed that prior research involvement strongly predicted audit knowledge (1–2 projects: aOR = 6.30; 3–4 projects: aOR = 4.92; p < 0.001).
Conclusions: Students expressed positive attitudes toward clinical audits but showed limited knowledge and very low participation. These findings highlight the need for structured, hands-on audit training within undergraduate medical curricula and improved institutional support to facilitate student engagement in quality improvement activities.
References
1. Smith R. Audit and research. BMJ. 1992;305(6859):905–6.
2. Burgess R, Moorhead J. New principles of best practice in clinical audit. Oxford: Radcliffe Publishing; 2011.
3. Kruk ME, Gage AD, Arsenault C, Jordan K, Leslie HH, Roder-DeWan S, et al. High-quality health systems in the Sustainable Development Goals era: time for a revolution. Lancet Glob Health. 2018;6(11):e1196–252.
4. Pirkle CM, Dumont A, Zunzunegui MV. Criterion-based clinical audit to assess quality of obstetrical care in low- and middle-income countries: a systematic review. Int J Qual Health Care. 2011;23(4):456–63.
5. Workumuluye WM, Tadesse S. Improving student participation in group project work: case study. Int J Educ Res. 2020;11(3):8–16. Available from: https://ijer.inased.org/makale/1661 Cited 2025 Dec 5.
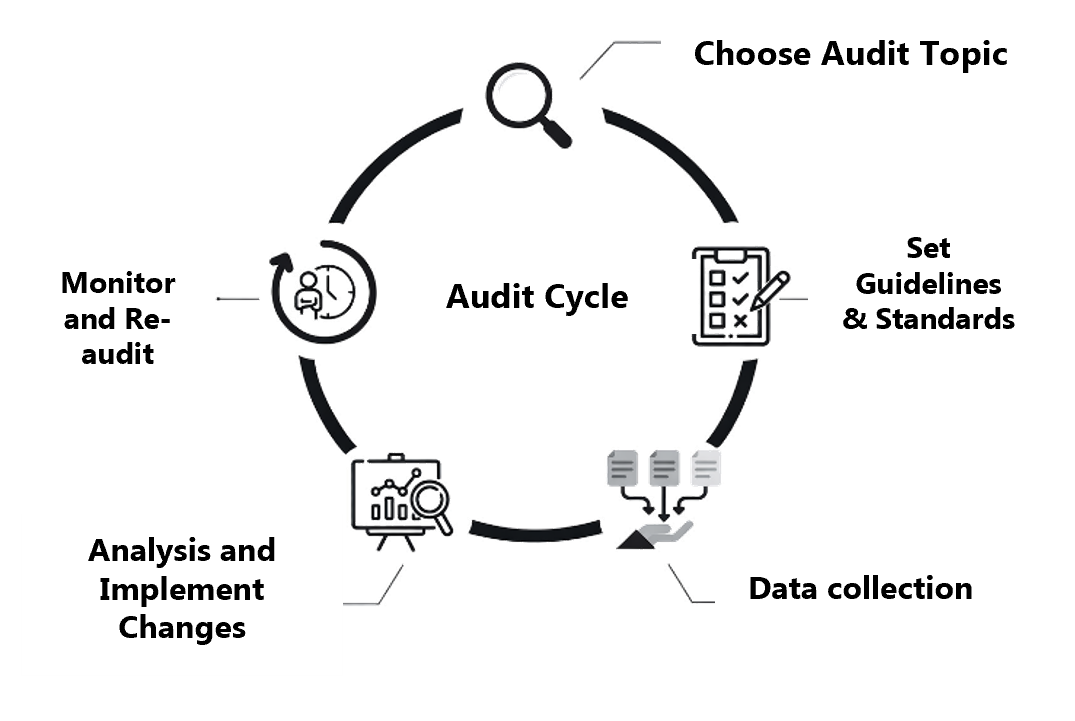
6. Takada T. Uncertainty in auditing. 2023. Available from: https://doi.org/10.53106/256299802023120501005 Cited 2025 Dec 5.
7. Narwani V, Nalamada K. Clinical audits: a realistic research opportunity for medical students. Med Teach. 2013;35(5):424.
8. Saravanan T, Shanmugapriya S. A study on the effectiveness of teaching the principles and methods of clinical audit to medical postgraduates. Curr Med Res Pract. 2018;8(2):59–63.
9. Davis S, O’Ferrall I, Hoare S, Caroline B, Mak DB. Perceptions of medical graduates and their workplace supervisors towards a medical school clinical audit program. Int J Med Educ. 2017;8:244–51.
10. Merry L, Castiglione SA, Rouleau G, Létourneau D, Larue C, Deschênes MF, et al. Continuing professional development (CPD) system development, implementation, evaluation and sustainability for healthcare professionals in low- and lower-middle-income countries: a rapid scoping review. BMC Med Educ. 2023;23(1):498.
11. Raosoft Inc. Sample size calculator. Available from: http://www.raosoft.com/samplesize.html Cited 2023 Oct 16.
12. The jamovi project. jamovi (Version 2.6) [computer software]. 2025. Available from: https://www.jamovi.org Cited 2025 Dec 5.
13. Desalu OO, Adeoti AO, Makusidi MA, Fadare JO, Aremu GO, Amao EA, et al. Family physicians/GP and internist opinions, familiarity and practice behaviour regarding clinical practice guidelines of common medical conditions in Nigeria. J Fam Med Prim Care. 2021;10(1):502–8.
14. Gillam S, Siriwardena AN. Frameworks for improvement: clinical audit, the plan-do-study-act cycle and significant event audit. Qual Prim Care. 2013;21(2):123–30.
15. Abu-Jeyyab M, Al-Jafari M, El Din Moawad MH, Alrosan S, Al Mse’adeen M. The role of clinical audits in advancing quality and safety in healthcare services: a multiproject analysis from a Jordanian hospital. Cureus. 2024. Available from: https://www.cureus.com/articles/220710-the-role-of-clinical-audits-in-advancing-quality-and-safety-in-healthcare-services-a-multiproject-analysis-from-a-jordanian-hospital Cited 2025 Dec 5.
16. Ravaghi H, Zarnaq RK, Adel A, Badpa M, Adel M, Abolhassani N. A survey on clinical governance awareness among clinical staff: a cross-sectional study. Glob J Health Sci. 2014;6(6):37–42.
17. Drake TM, Bath M, Claireaux H, Mohan M, Fitzgerald JEF, Dynes K, et al. Medical research and audit skills training for undergraduates: an international analysis and student-focused needs assessment. Postgrad Med J. 2018;94(1107):37–42.
Downloads
Published
How to Cite
License
Copyright (c) 2025 Mohammad Ghassab Deameh, Omar S Mansour, Hammam Abu Rahmeh, Baha’ Aldeen Bani Irshid, Mohammad Walid Da'meh, Enas A. Amaireh, Yazeed Badran, Jebreen A. Elaydi, Hasan M. Abu Obaideh, Suhaib Feras Fawarseh, Khaled Funjan

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- The Author retains copyright in the Work, where the term “Work” shall include all digital objects that may result in subsequent electronic publication or distribution.
- Upon acceptance of the Work, the author shall grant to the Publisher the right of first publication of the Work.
- The Author shall grant to the Publisher and its agents the nonexclusive perpetual right and license to publish, archive, and make accessible the Work in whole or in part in all forms of media now or hereafter known under a Creative Commons Attribution 4.0 International License or its equivalent, which, for the avoidance of doubt, allows others to copy, distribute, and transmit the Work under the following conditions:
- Attribution—other users must attribute the Work in the manner specified by the author as indicated on the journal Web site; with the understanding that the above condition can be waived with permission from the Author and that where the Work or any of its elements is in the public domain under applicable law, that status is in no way affected by the license.
- The Author is able to enter into separate, additional contractual arrangements for the nonexclusive distribution of the journal's published version of the Work (e.g., post it to an institutional repository or publish it in a book), as long as there is provided in the document an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post online a prepublication manuscript (but not the Publisher’s final formatted PDF version of the Work) in institutional repositories or on their Websites prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. Any such posting made before acceptance and publication of the Work shall be updated upon publication to include a reference to the Publisher-assigned DOI (Digital Object Identifier) and a link to the online abstract for the final published Work in the Journal.
- Upon Publisher’s request, the Author agrees to furnish promptly to Publisher, at the Author’s own expense, written evidence of the permissions, licenses, and consents for use of third-party material included within the Work, except as determined by Publisher to be covered by the principles of Fair Use.
- The Author represents and warrants that:
- the Work is the Author’s original work;
- the Author has not transferred, and will not transfer, exclusive rights in the Work to any third party;
- the Work is not pending review or under consideration by another publisher;
- the Work has not previously been published;
- the Work contains no misrepresentation or infringement of the Work or property of other authors or third parties; and
- the Work contains no libel, invasion of privacy, or other unlawful matter.
- The Author agrees to indemnify and hold Publisher harmless from the Author’s breach of the representations and warranties contained in Paragraph 6 above, as well as any claim or proceeding relating to Publisher’s use and publication of any content contained in the Work, including third-party content.
Enforcement of copyright
The IJMS takes the protection of copyright very seriously.
If the IJMS discovers that you have used its copyright materials in contravention of the license above, the IJMS may bring legal proceedings against you seeking reparation and an injunction to stop you using those materials. You could also be ordered to pay legal costs.
If you become aware of any use of the IJMS' copyright materials that contravenes or may contravene the license above, please report this by email to contact@ijms.org
Infringing material
If you become aware of any material on the website that you believe infringes your or any other person's copyright, please report this by email to contact@ijms.org







