Empathy in Practice: Comparing Physicians’ Self-Assessment and Patient Perceptions Using the Jefferson Scales
DOI:
https://doi.org/10.5195/ijms.2025.3247Keywords:
Empathy, Medical education, Jefferson scale, Physician and patient empathy, Cross-Sectional Study, South India, Communication Skills, Jefferson Scale of Physician Empathy, Patient Perception, PPPE; Doctor–Patient RelationshipAbstract
Background: Empathy is essential for effective patient care, improving communication, satisfaction, and compliance. This study was done to assess empathy levels in a tertiary care center in South India.
Materials and Methods: A cross-sectional study among 40 physicians from various specialties assessed physician empathy using the Jefferson Scale of Physician Empathy–Health Professionals version (JSE-HP) and patient perceptions using the Jefferson Scale of Patient Perceptions of Physician Empathy (JSPPPE). Five patients per physician participated. Data were collected from January to June 2024, and was analyzed by a t-paired and ANOVA tests and a multilevel linear mixed-effects model.
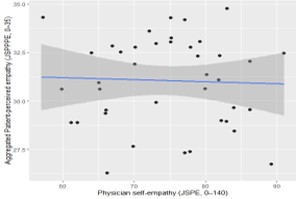
Results: A total of 200 patient–physician encounters were analyzed. Most physicians were under 50 years (90%), and patients were aged 19–85 years. Mean physician self-empathy (JSE) was 74.5 ± 8.6, and mean patient-perceived empathy (JSPPPE) was 31.0 ± 4.6. No correlation was observed between self- and patient-rated empathy (ρ = −0.06, p = 0.71). In multilevel analysis, self-empathy was not associated with patient-perceived empathy (β = −0.05, 95% CI [−0.15, 0.06], p = 0.37). Physician age, gender, and specialty were not significant predictors. The intraclass correlation coefficient (ICC = 0.066) indicated 7% of variance in patient empathy scores was due to physician-level differences.
Conclusion: A disparity exists between physicians’ self-perceived and patient-rated empathy. Experienced physicians and those in patient-centered specialties are rated higher. Regular empathy training and feedback can align self-perceptions with patient expectations, improving communication and care quality.
References
1. Riess H. The science of empathy. J Patient Exp. 2017;4(2):74–7.
2. Perry A, Shamay-Tsoory S. Understanding emotional and cognitive empathy: a neuropsychological perspective. In: Baron-Cohen S, Tager-Flusberg H, Lombardo MV, editors. Understanding other minds. 3rd ed. Oxford: Oxford Univ Press; 2013. p. 178–94.
3. Klöckner CC, Gerbase MW, Nendaz M, Baroffio A, Junod NP. Relationship between self-reported cognitive and behavioural empathy among medical students. Patient Educ Couns. 2022;105(4):895–901.
4. Segal EA. Social empathy: a model built on empathy, contextual understanding, and social responsibility that promotes social justice. J Soc Serv Res. 2011;37(3):266–77.
5. Figueredo AJ, Steklis NG, Peñaherrera-Aguirre M, Fernandes HBF, de Baca TC, Salmon C, et al. The influence of individual differences and local ecological conditions on emotional empathy, cognitive empathy, and harm avoidance towards nonhuman animals. Hum Anim Interact. 2022;2022:0021.
6. Gerace A, Day A, Casey S, Mohr P. An exploratory investigation of the process of perspective taking in interpersonal situations. J Relatsh Res. 2013;4:e6.
7. Moudatsou M, Stavropoulou A, Philalithis A, Koukouli S. The role of empathy in health and social care professionals. Healthcare (Basel). 2020;8(1):26.
8. Sturzu L, Lala A, Bisch M, Guitter M, Dobre D, Schwan R. Empathy and burnout: a cross-sectional study among mental healthcare providers in France. J Med Life. 2019;12(1):21–9.
9. Moya-Salazar J, Goicochea-Palomino EA, Porras-Guillermo J, Cañari B, Jaime-Quispe A, Zuñiga N, et al. Assessing empathy in healthcare services: a systematic review of South American healthcare workers’ and patients’ perceptions. Front Psychiatry. 2023;14:1249620.
10. He S, Sultana R, Anantham D, Loh HP, Zhou JX, Tang JY, et al. Empathy levels among healthcare professionals: an Asian multi-professional cross-sectional study. Cureus. 2024;16(2):e53750.
11. Howick J, Steinkopf L, Ulyte A, Roberts N, Meissner K. How empathic is your healthcare practitioner? A systematic review and meta-analysis of patient surveys. BMC Med Educ. 2017;17(1):136.
12. Hermans L, Olde Hartman TC, Dielissen PW. Differences between GP perception of delivered empathy and patient-perceived empathy: a cross-sectional study in primary care. Br J Gen Pract. 2018;68(674):e621–6.
13. Nasiri M, Amini M, Mani A, Delavari S, Kiani M, Sagheb MM, et al. Assessing empathy in final-year medical students using the Persian version of the Jefferson Scale of Physician Empathy. J Educ Health Promot. 2021;10:310.
14. Tonelli M, Wiebe N, Manns BJ, Klarenbach SW, James MT, Ravani P, et al. Comparison of the complexity of patients seen by different medical subspecialists in a universal health care system. JAMA Netw Open. 2018;1(7):e184852.
15. Hojat M. Empathy in health professions education and patient care. New York: Springer Int Publ; 2016.
16. Hojat M, Gonnella JS, Nasca TJ, Mangione S, Veloski JJ, Magee M, et al. The Jefferson Scale of Physician Empathy: further psychometric data and differences by gender and specialty at item level. Acad Med. 2002;77(10 Suppl):S58–60.
17. Hojat M, Maio V, Pohl CA, et al. Clinical empathy: definition, measurement, correlates, group differences, erosion, enhancement, and healthcare outcomes. Discov Health Syst. 2023;2:8.
18. Gathara D, English M, van Hensbroek MB, et al. Exploring sources of variability in adherence to guidelines across hospitals in low-income settings: a multi-level analysis of a cross-sectional survey of 22 hospitals. Implement Sci. 2015;10:60.
19. Krol MW, de Boer D, Rademakers JJ, et al. Overall scores as an alternative to global ratings in patient experience surveys: a comparison of four methods. BMC Health Serv Res. 2013;13:479.
20. Bernardo MO, Cecílio-Fernandes D, Costa P, Quince TA, Costa MJ, Carvalho-Filho MA. Physicians’ self-assessed empathy levels do not correlate with patients’ assessments. PLoS One. 2018;13(5):e0198488.
21. Akham N, Goutam S, Rajkumari J, Singh TA, Singh TA. Physicians’ empathy toward patients at a private medical college, Manipur: a cross-sectional study. Int J Community Med Public Health. 2025;12(4):1742–7.
22. Wang H, Kline JA, Jackson BE, Laureano-Phillips J, Robinson RD, Cowden CD, et al. Association between emergency physician self-reported empathy and patient satisfaction. PLoS One. 2018;13(9):e0204113.
23. Park C, Lee YJ, Hong M, Jung CH, Synn Y, Kwack YS, et al. A multicenter study investigating empathy and burnout characteristics in medical residents with various specialties. J Korean Med Sci. 2016;31(4):590–7.
24. Walocha E, Tomaszewska IM, Mizia E. Empathy level differences between Polish surgeons and physicians. Folia Med Cracov. 2013;53(1):47–54.
25. Abdulkader RS, Venugopal D, Jeyashree K, Al Zayer Z, Senthamarai Kannan K, Jebitha R, et al. The intricate relationship between client perceptions of physician empathy and physician self-assessment: lessons for reforming clinical practice. J Patient Exp. 2022;9:23743735221077537.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Eliz Thomas, Shwetha Shenod, Bhavana Madhu, Sibivishal SR, Robin S

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- The Author retains copyright in the Work, where the term “Work” shall include all digital objects that may result in subsequent electronic publication or distribution.
- Upon acceptance of the Work, the author shall grant to the Publisher the right of first publication of the Work.
- The Author shall grant to the Publisher and its agents the nonexclusive perpetual right and license to publish, archive, and make accessible the Work in whole or in part in all forms of media now or hereafter known under a Creative Commons Attribution 4.0 International License or its equivalent, which, for the avoidance of doubt, allows others to copy, distribute, and transmit the Work under the following conditions:
- Attribution—other users must attribute the Work in the manner specified by the author as indicated on the journal Web site; with the understanding that the above condition can be waived with permission from the Author and that where the Work or any of its elements is in the public domain under applicable law, that status is in no way affected by the license.
- The Author is able to enter into separate, additional contractual arrangements for the nonexclusive distribution of the journal's published version of the Work (e.g., post it to an institutional repository or publish it in a book), as long as there is provided in the document an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post online a prepublication manuscript (but not the Publisher’s final formatted PDF version of the Work) in institutional repositories or on their Websites prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. Any such posting made before acceptance and publication of the Work shall be updated upon publication to include a reference to the Publisher-assigned DOI (Digital Object Identifier) and a link to the online abstract for the final published Work in the Journal.
- Upon Publisher’s request, the Author agrees to furnish promptly to Publisher, at the Author’s own expense, written evidence of the permissions, licenses, and consents for use of third-party material included within the Work, except as determined by Publisher to be covered by the principles of Fair Use.
- The Author represents and warrants that:
- the Work is the Author’s original work;
- the Author has not transferred, and will not transfer, exclusive rights in the Work to any third party;
- the Work is not pending review or under consideration by another publisher;
- the Work has not previously been published;
- the Work contains no misrepresentation or infringement of the Work or property of other authors or third parties; and
- the Work contains no libel, invasion of privacy, or other unlawful matter.
- The Author agrees to indemnify and hold Publisher harmless from the Author’s breach of the representations and warranties contained in Paragraph 6 above, as well as any claim or proceeding relating to Publisher’s use and publication of any content contained in the Work, including third-party content.
Enforcement of copyright
The IJMS takes the protection of copyright very seriously.
If the IJMS discovers that you have used its copyright materials in contravention of the license above, the IJMS may bring legal proceedings against you seeking reparation and an injunction to stop you using those materials. You could also be ordered to pay legal costs.
If you become aware of any use of the IJMS' copyright materials that contravenes or may contravene the license above, please report this by email to contact@ijms.org
Infringing material
If you become aware of any material on the website that you believe infringes your or any other person's copyright, please report this by email to contact@ijms.org







