A Reflective Case Study: Complex Presentation of a Veteran Patient with Cardiomyopathy and a History of Facial Reconstruction
DOI:
https://doi.org/10.5195/ijms.2025.3498Keywords:
veteran health, Trauma-informed care, cardiomyopathy, denial, facial trauma, non-adherence, Cardiomyopathies, Cardiomyopathy, Cardiovascular Diseases, War-Related InjuriesAbstract
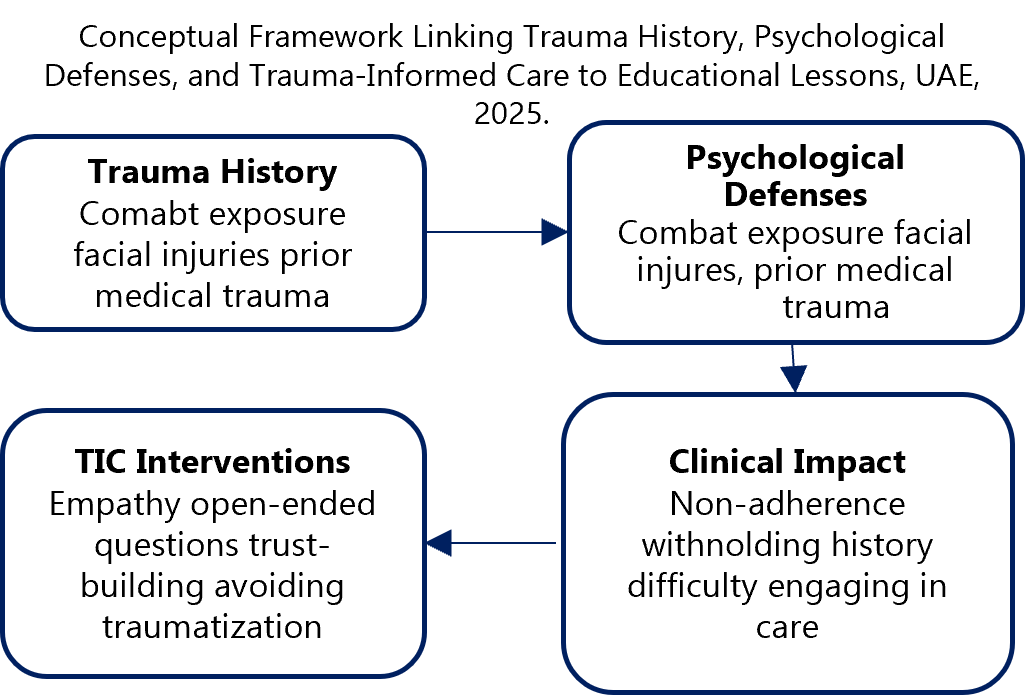
Trauma-informed care (TIC) reframes complex patient encounters by recognizing the lasting impact of trauma on health behaviors. I describe the case of a male veteran in his sixties who presented with apparent gastrointestinal illness, yet further evaluation revealed untreated cardiomyopathy and a history of combat-related facial reconstruction. Despite clear evidence, the patient denied his cardiac condition, reflecting mistrust of healthcare and the psychological burden of trauma. This denial complicated diagnostic reasoning and care planning but underscored the critical role of TIC in uncovering hidden narratives behind clinical presentations. By shifting focus from symptoms to context, this case highlights how trauma, resilience, and denial intersect in medical practice. It calls for reflective approaches that integrate psychosocial insight into clinical decision-making, particularly when caring for veterans and patients with complex life histories.
References
1. Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure. J Am Coll Cardiol. 2013. Available from: https://www.acc.org/Latest-in-Cardiology/Journal-Scans/2013/06/06/16/29/2013-ACCF-AHA-Guideline-for-the-Management-of-Heart-Failure. Cited 2025 Aug 19.
2. Moser DK, Watkins JF. Conceptualizing self-care in heart failure: a life course model of patient characteristics. J Cardiovasc Nurs. 2008 Available from: https://pubmed.ncbi.nlm.nih.gov/18437061/. Cited 2025 Aug 19.
3. Glaesmer H, Brähler E, Gündel H, Riedel-Heller SG. The association of traumatic experiences and posttraumatic stress disorder with physical morbidity in older age. Psychol Med. 2011. Available from: https://pubmed.ncbi.nlm.nih.gov/21636658/. Cited 2025 Aug 19.
4. Lew TA, Walker JA, Wenke JC, Blackbourne LH, Hale RG. Characterization of craniomaxillofacial battle injuries sustained by United States service members in the current conflicts of Iraq and Afghanistan. J Oral Maxillofac Surg. 2010. Available from: https://pubmed.ncbi.nlm.nih.gov/20006147/. Cited 2025 Aug 19.
5. Kaufman MR, Bell TM, Hunsberger JB, O’Rourke PP. Psychological effects of facial trauma: implications for acute care. J Trauma Nurs. 2013. Available from: https://journals.lww.com/jtraumanurs/Abstract/2013/05000/Psychological_Effects_of_Facial_Trauma__Implications.6.aspx. Cited 2025 Aug 19.
6. Seal KH, Bertenthal D, Miner CR, Sen S, Marmar C. Bringing the war back home: mental health disorders among 103,788 US veterans returning from Iraq and Afghanistan seen at Department of Veterans Affairs facilities. Arch Intern Med. 2007. Available from: https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/769661. Cited 2025 Aug 19.
7. Substance Abuse and Mental Health Services Administration. Trauma-informed care in behavioral health services. Treatment Improvement Protocol (TIP) Series 57. Rockville (MD): SAMHSA; 2014. Available from: https://store.samhsa.gov/product/TIP-57-Trauma-Informed-Care-in-Behavioral-Health-Services/SMA13-4801. Cited 2025 Aug 19.
8. DiMatteo MR. Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004; from: https://pubmed.ncbi.nlm.nih.gov/15076819/. Cited 2025 Aug 19.
9. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington (VA): American Psychiatric Association; 2013. Available from: https://www.psychiatry.org/psychiatrists/practice/dsm. Cited 2025 Aug 19.
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2025 Zainab AL-Rubaiy

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- The Author retains copyright in the Work, where the term “Work” shall include all digital objects that may result in subsequent electronic publication or distribution.
- Upon acceptance of the Work, the author shall grant to the Publisher the right of first publication of the Work.
- The Author shall grant to the Publisher and its agents the nonexclusive perpetual right and license to publish, archive, and make accessible the Work in whole or in part in all forms of media now or hereafter known under a Creative Commons Attribution 4.0 International License or its equivalent, which, for the avoidance of doubt, allows others to copy, distribute, and transmit the Work under the following conditions:
- Attribution—other users must attribute the Work in the manner specified by the author as indicated on the journal Web site; with the understanding that the above condition can be waived with permission from the Author and that where the Work or any of its elements is in the public domain under applicable law, that status is in no way affected by the license.
- The Author is able to enter into separate, additional contractual arrangements for the nonexclusive distribution of the journal's published version of the Work (e.g., post it to an institutional repository or publish it in a book), as long as there is provided in the document an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post online a prepublication manuscript (but not the Publisher’s final formatted PDF version of the Work) in institutional repositories or on their Websites prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. Any such posting made before acceptance and publication of the Work shall be updated upon publication to include a reference to the Publisher-assigned DOI (Digital Object Identifier) and a link to the online abstract for the final published Work in the Journal.
- Upon Publisher’s request, the Author agrees to furnish promptly to Publisher, at the Author’s own expense, written evidence of the permissions, licenses, and consents for use of third-party material included within the Work, except as determined by Publisher to be covered by the principles of Fair Use.
- The Author represents and warrants that:
- the Work is the Author’s original work;
- the Author has not transferred, and will not transfer, exclusive rights in the Work to any third party;
- the Work is not pending review or under consideration by another publisher;
- the Work has not previously been published;
- the Work contains no misrepresentation or infringement of the Work or property of other authors or third parties; and
- the Work contains no libel, invasion of privacy, or other unlawful matter.
- The Author agrees to indemnify and hold Publisher harmless from the Author’s breach of the representations and warranties contained in Paragraph 6 above, as well as any claim or proceeding relating to Publisher’s use and publication of any content contained in the Work, including third-party content.
Enforcement of copyright
The IJMS takes the protection of copyright very seriously.
If the IJMS discovers that you have used its copyright materials in contravention of the license above, the IJMS may bring legal proceedings against you seeking reparation and an injunction to stop you using those materials. You could also be ordered to pay legal costs.
If you become aware of any use of the IJMS' copyright materials that contravenes or may contravene the license above, please report this by email to contact@ijms.org
Infringing material
If you become aware of any material on the website that you believe infringes your or any other person's copyright, please report this by email to contact@ijms.org







