Enhancing Medical Education: The Impact of Deliberate Practice on Learning Human Physiology
DOI:
https://doi.org/10.5195/ijms.2024.2284Keywords:
Simulation, Medical Education, PhysiologyAbstract
Background: Simulation-Based Learning (SBL) has potential in health education, yet it remains underutilized at the undergraduate level. Active teaching methodologies, such as deliberate practice, are known to enhance skills like leadership, self-confidence, and teamwork. This study aimed to evaluate the medical students’ perception of deliberate practice in learning Human Physiology at a private medical school in Brazil.
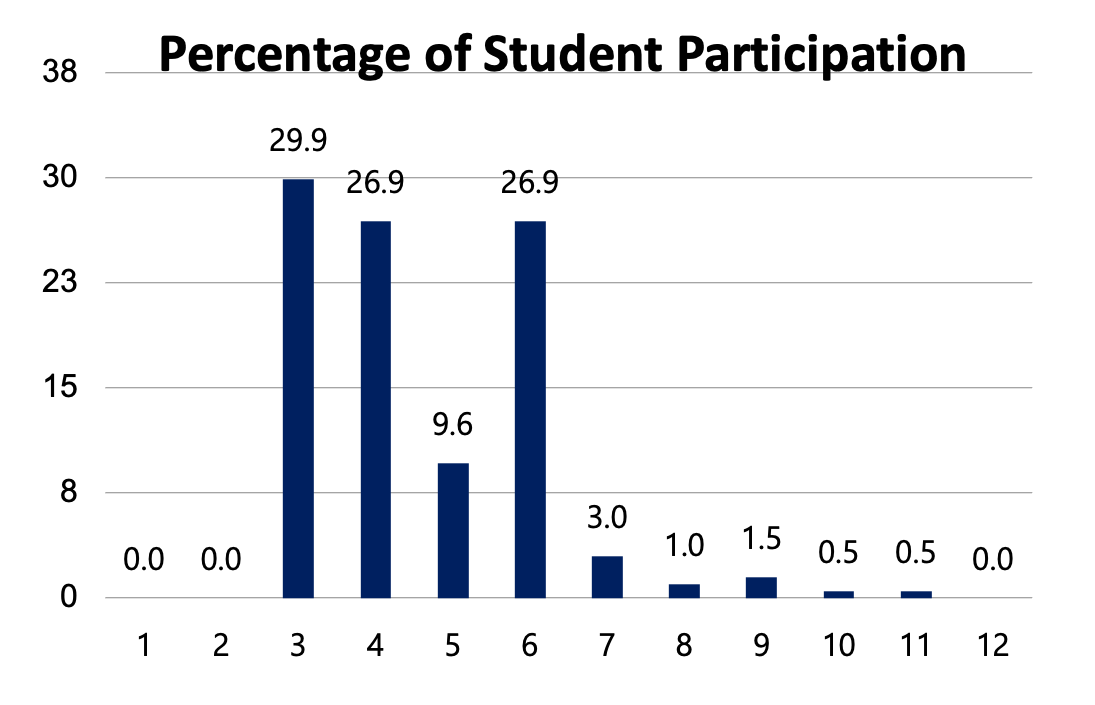
Methods: An observational qualitative and quantitative study was conducted in 2022 and 2023 using an online questionnaire, including 198 participants. An inferential statistical analysis was conducted, using Fisher's exact test at a 0.05 level of significance, to assess the association between categorical variables.
Results: Overall, students had a positive perception of deliberate practice. A significant proportion (66.8%) strongly agreed that they developed teamwork skills through the scenarios. Additionally, 83.7% strongly agreed that access to realistic simulation environments enhanced their learning. In terms of emotions, 67.9% felt motivated, while 37.8% experienced anxiety during the scenarios. The statistical analysis revealed a significant association between the sum scores of each section and the binary response (“yes” or “no”) to the question “Do you like the practical classes of Human Physiology?” (p < 0.05), with the exception of the Negative Emotions sum. This indicates that higher section scores are associated with a greater likelihood of students liking the practical classes.
Conclusion: The integration of deliberate practice into the Human Physiology curriculum has positively impacted students’ learning and skill development. However, enhancements are needed to create a safer emotional environment for students.
References
Filho A, Scarpelini S. [SIMULATION: DEFINITION]. Rev USP. 2007 Apr.
Herrera-Aliaga E, Estrada LD. Trends and Innovations of Simulation for Twenty First Century Medical Education. Front Public Health. 2022 Mar 3;10.
Dufrene C, Young A, et al. Successful debriefing — Best methods to achieve positive learning outcomes: A literature review. Nurse Educ Today. 2014 Mar;34(3):372–6. Portuguese.
Ross S. Twelve tips for effective simulation debriefing: A research-based approach. Med Teach. 2020 Oct 14;43(6):1–4.
Nascimento J da SG, Pires FC, Castro JPR, Nascimento KG do, Oliveira JLG de, Dalri MCB. [Instructor-led oral debriefing technique in clinical nursing simulation: integrative review]. Rev Bras Enferm. 2021;74(suppl 5). Portuguese.
Henrico K, Oostdam N. Promoting critical thinking through simulation-based healthcare training (SBHT): A scoping review. Afr J Health Prof Educ. 2022 Nov 23;160–4.
Paula A, Giovana M, Quint FC, Pereira AL, Bueno U. [Communicating Bad News with Standard-ized Patients: A Teaching Strategy for Medical Students]. Rev bras educ med. 2021 Jun 11;45. Portuguese.
Ericsson KA. The Role of Deliberate Practice in the Acquisition of Expert Performance. Re-searchGate. 1993.
Ferreira C. IMPACT OF REALISTIC SIMULATION METHODOLOGY AS A TECHNOLOGY AP-PLIED TO EDUCATION IN HEALTH COURSES. Anais do Seminário Tecnologias Aplicadas a Educação e Saúde. Rev UNEB. 2015;32(1):S32-40.
Fukamizu J, Verstegen D, Ho SC. International trainer perceptions of simulation-based learning: a qualitative study. Int J Med Educ. 2021 Dec 27;12:267–73.
Dreifuerst KT. Using Debriefing for Meaningful Learning to Foster Development of Clinical Rea-soning in Simulation. J Nurs Educ. 2012 Apr 9;51(6):326–33.
Madsgaard A, Smith‐Strøm H, Hunskår I, Røykenes K. A rollercoaster of emotions: An integra-tive review of emotions and its impact on health professional students’ learning in simulation‐based educa-tion. Nurs Open. 2021 Oct 21;9(1):108–21.
Mulyadi M, Tonapa SI, Rompas SSJ, Wang RH, Lee BO. Effects of simulation technology-based learning on nursing students’ learning outcomes: A systematic review and meta-analysis of experi-mental studies. Nurse Educ Today. 2021 Dec;107:105127.
Sheikhbardsiri H, Sheikhasadi H, Mahani SA, Mohamadi MMD. Emotional intelligence and learn-ing strategies of postgraduate students at Kerman University of Medical Sciences in the southeast of Iran. J Educ Health Promot. 2020 Mar 3;9:66.
Córdova A, Caballero-García A, Drobnic F, Roche E, Noriega DC. Influence of Stress and Emo-tions in the Learning Process: The Example of COVID-19 on University Students: A Narrative Review. Healthcare (Basel). 2023 Jun 17;11(12):1787.
Luiz Thomaz De Souza A, Passaglia P, Cárnio E. [Use of High Fidelity Realistic Simulator in the Teaching of Human Physiology in the Nursing Course]. Rev Grad USP. 2018;3(2). Portuguese.
Bolfarine H, de W De B. [Sampling Elements]. São Paulo: Edgard Blücher; 2007. Portuguese.
Teixeira CR de S, Pereira MCA, Kusumota L, Gaioso VP, Mello CL de, Carvalho EC de. [Evalua-tion of nursing students on learning from clinical simulation]. Rev Bras Enferm. 2015 Apr;68(2):311–9. Portu-guese.
Dourado ASS, Giannella TR. [Simulation-based teaching in the continuing education of physi-cians: analysis of the perceptions of students and professors of a hospital in Rio de Janeiro]. Rev Bras Educ Med. 2014 Dec;38(4):460–9. Portuguese.
Simon R, Raemer DB, Rudolph JW, et al. Debriefing Assessment for Simulation in Healthcare (DASH)© – Student Version. Boston: Center for Medical Simulation; 2010.
Duvivier RJ, van Dalen J, Muijtjens AM, Moulaert VR, van der Vleuten CP, Scherpbier AJ. The role of deliberate practice in the acquisition of clinical skills. BMC Med Educ [Internet]. 2011 Dec [cited 2019 Nov 21];11(1). Available from: https://bmcmededuc.biomedcentral.com/articles/10.1186/1472-6920-11-101
Toufan N, Omid A, Haghani F. The double-edged sword of emotions in medical education: A scoping review. J Educ Health Promot [Internet]. 2023 [cited 2023 Sep 9];12:52. Available from: https://pubmed.ncbi.nlm.nih.gov/37113412/
Yu JH, Chang HJ, Kim SS, Park JE, Chung WY, Lee SK, et al. Effects of high-fidelity simulation education on medical students’ anxiety and confidence. PLoS One. 2021;16(5):e0251429.
Schaefer A, Mattheß H, Pfitzer G, Köhle K. [Mental health and performance of medical students with high and low test anxiety]. Psychother Psychosom Med Psychol. 2007 Jul;57(7):289–97. German.
Bresolin P, Martini JG, Maffissoni AL, Sanes M da S, Riegel F, Unicovsky MAR. [Debriefing in clinical nursing simulation: an analysis based on the theory of experiential learning]. Rev Gaúcha Enferm. 2022;43:e20220154. Portuguese.
Keskitalo T, Ruokamo H. Exploring learners’ emotions and emotional profiles in simulation-based medical education. Australas J Educ Technol. 2021;37(6):15–26.
Published
Versions
- 2025-01-05 (3)
- 2024-12-16 (2)
How to Cite
License
Copyright (c) 2024 Júlia Silva Souza, Lavínia Penido Safe, Airton Martins da Costa Lopes, Augusto Scalabrini - Neto

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- The Author retains copyright in the Work, where the term “Work” shall include all digital objects that may result in subsequent electronic publication or distribution.
- Upon acceptance of the Work, the author shall grant to the Publisher the right of first publication of the Work.
- The Author shall grant to the Publisher and its agents the nonexclusive perpetual right and license to publish, archive, and make accessible the Work in whole or in part in all forms of media now or hereafter known under a Creative Commons Attribution 4.0 International License or its equivalent, which, for the avoidance of doubt, allows others to copy, distribute, and transmit the Work under the following conditions:
- Attribution—other users must attribute the Work in the manner specified by the author as indicated on the journal Web site; with the understanding that the above condition can be waived with permission from the Author and that where the Work or any of its elements is in the public domain under applicable law, that status is in no way affected by the license.
- The Author is able to enter into separate, additional contractual arrangements for the nonexclusive distribution of the journal's published version of the Work (e.g., post it to an institutional repository or publish it in a book), as long as there is provided in the document an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post online a prepublication manuscript (but not the Publisher’s final formatted PDF version of the Work) in institutional repositories or on their Websites prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. Any such posting made before acceptance and publication of the Work shall be updated upon publication to include a reference to the Publisher-assigned DOI (Digital Object Identifier) and a link to the online abstract for the final published Work in the Journal.
- Upon Publisher’s request, the Author agrees to furnish promptly to Publisher, at the Author’s own expense, written evidence of the permissions, licenses, and consents for use of third-party material included within the Work, except as determined by Publisher to be covered by the principles of Fair Use.
- The Author represents and warrants that:
- the Work is the Author’s original work;
- the Author has not transferred, and will not transfer, exclusive rights in the Work to any third party;
- the Work is not pending review or under consideration by another publisher;
- the Work has not previously been published;
- the Work contains no misrepresentation or infringement of the Work or property of other authors or third parties; and
- the Work contains no libel, invasion of privacy, or other unlawful matter.
- The Author agrees to indemnify and hold Publisher harmless from the Author’s breach of the representations and warranties contained in Paragraph 6 above, as well as any claim or proceeding relating to Publisher’s use and publication of any content contained in the Work, including third-party content.
Enforcement of copyright
The IJMS takes the protection of copyright very seriously.
If the IJMS discovers that you have used its copyright materials in contravention of the license above, the IJMS may bring legal proceedings against you seeking reparation and an injunction to stop you using those materials. You could also be ordered to pay legal costs.
If you become aware of any use of the IJMS' copyright materials that contravenes or may contravene the license above, please report this by email to contact@ijms.org
Infringing material
If you become aware of any material on the website that you believe infringes your or any other person's copyright, please report this by email to contact@ijms.org







